Laparoscopic enucleation of solitary pancreatic insulinoma in Al Najaf City in Iraq (Sep.2017)
Abstract
Insulinomas are the most common cause of hypoglycemia resulting from endogenous hyperinsulinism.We reported two cases with pancreatic insulinoma. The first one in a 47 years old male with a 21×20 mm insulinoma localized between body and tail of the pancreas; the second one in a 30 years old female with a 7 mm insulinoma localized at the middle of pancreatic body. In both cases, the tumor was removed by laparoscopic enucleation in August 2017 in Al-Najaf city, Iraq. In the postoperative period of both cases, the blood glucose level and insulin level returned to normal.
Introduction
Insulinoma are the most common functional pancreatic endocrine neoplasm, and present with typical clinical syndrome known as Whipple’s triad. Patient can be presented with profound syncopal attack or less severe symptoms that are averted by frequent eating.
Common symptoms include palpitation, trembling, diaphoresis, confusion, and seizure. The family may report that the patient has undergone personal changes.
Diagnosis is by signs and symptoms, close monitoring of the patient in the ward for 72 hours, and checking fasting blood sugar every 4-6 hours, and when the patient becomes symptomatic, we check insulin level and c-peptide to rule out exogenous insulin and other hypoglycemic agents.
After clinching the diagnosis, we should localize the mass, which is best done by CT scan and EUS. Visceral angiography with venous sampling is rarely used to accurately localize the tumor.
The majority of insulinoma are benign and solitary (>90%). Only 10% are malignant. The tumor is eitherapproached by open resection or laparoscopic simple enucleation. Tumors located close the pancreatic duct that are >2 cm in size may require distal pancreatectomy or Whipple’s procedure. Intraoperative ultrasound is used to determine the tumor relation to the main pancreatic duct, and is used as a guide for intraoperative decision making.
Approximately 90% of insulinoma are sporadic and 10% associated with MEN I syndrome. Those associated with MENI syndrome are usually multifocal with high rate of recurrence.
Case presentation
We report two cases of insulinoma enucleation done by laparoscopic surgery (minimally invasive technique)
Case 1:
47 years old male presented with recurrent syncopal attacks, palpitations, diaphoresis, with recurrent fall of blood glucose level below 50 mg/dl. Physical examination was unremarkable.
Investigations showed randum blood sugar below 50 mg/dl, insulin level 98.2 u/L, c-peptide 6.9 u/L, and the patient was diagnosed with insulinoma.
Localization of the mass was done by CT scan with IV contrast, which revealed well avid enhancing mass measuring 21×20 mm between body and tail of the pancreas.
CTscan show pancreatic mass case1
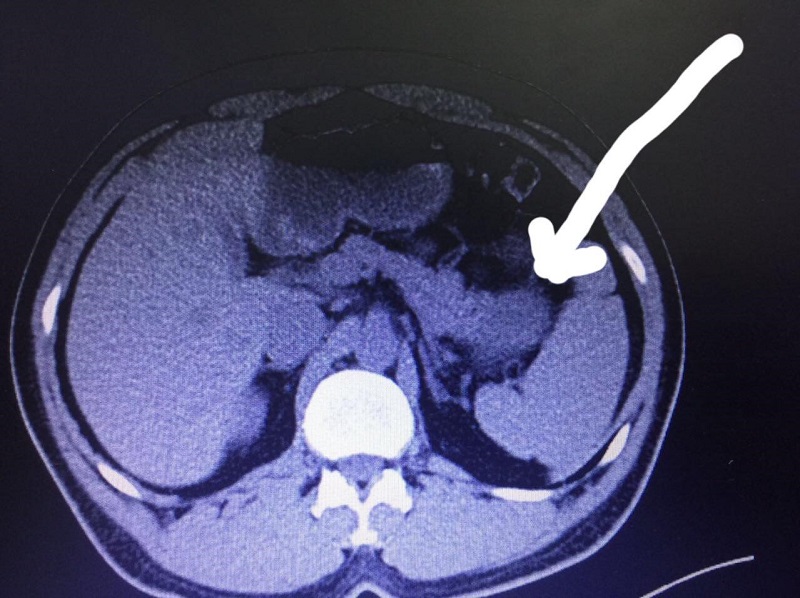
CTscan show pancreatic mass case1
The patient was admitted to the ward 24 hours before surgery and was put on hypertonic glucose infusion and glucose monitoring every 4 hours. He was put on nill per os 8 hours before surgery with blood glucose monitoring every 4 hours.
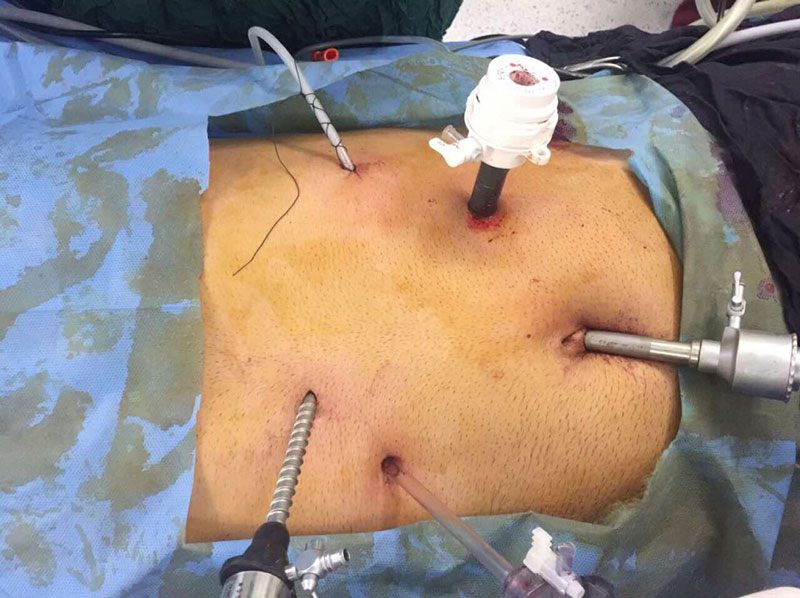
The operation was done under general anasthesia, supine position, with four ports incision. We opened the lesser sac,the stomach was retracted upward, dissected the pancreatic mass at tail of pancreas by using ligasure. The surgery was uneventful. We put a drain in the lesser sac. The operating time was 90 minutes.
postion of ports of laparoscopy case1
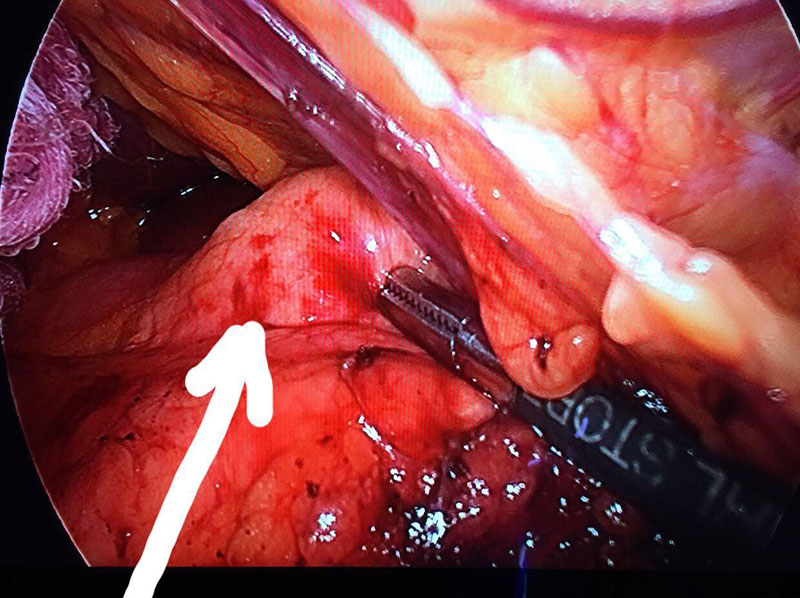
picture show the mass grasped case1
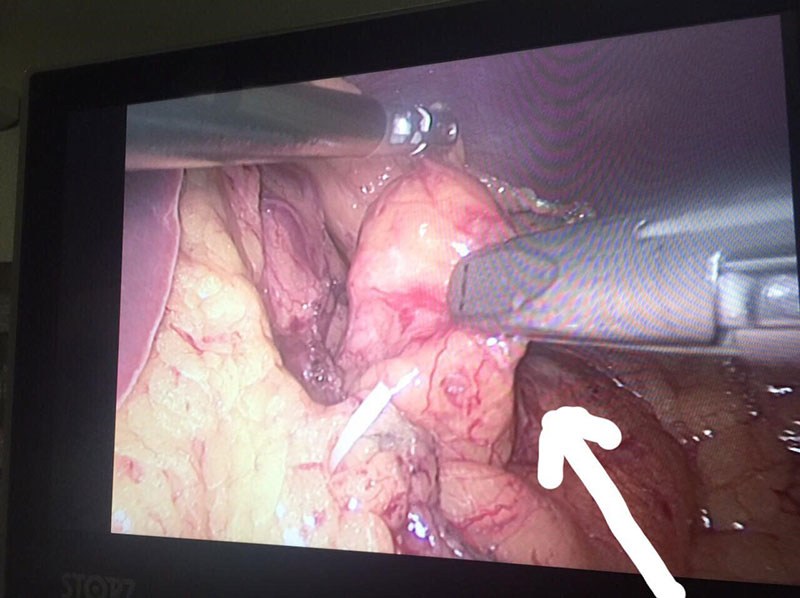
pancreatic mass dissection case1
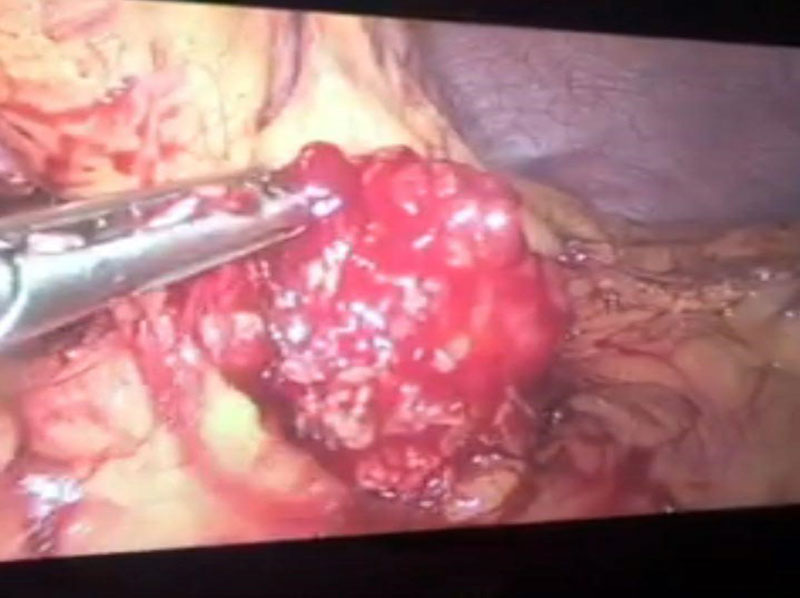
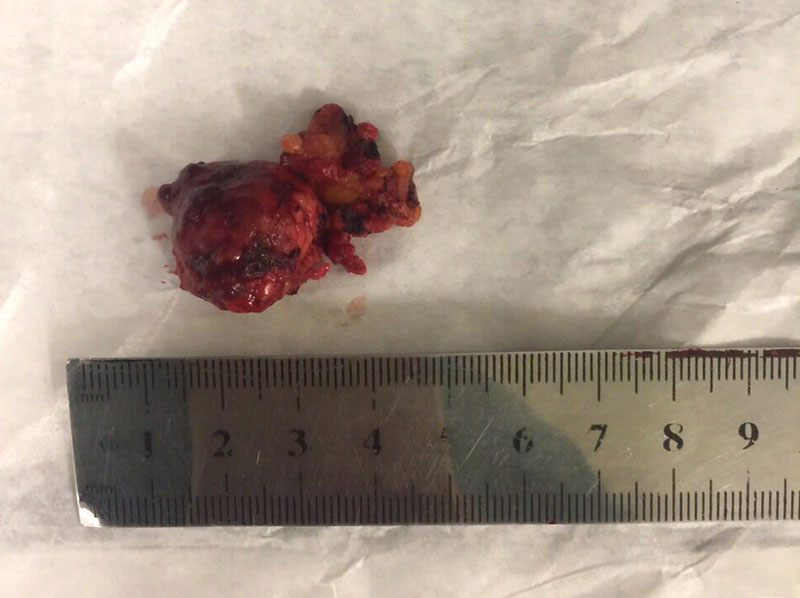
the mass completly enucleated case1
Postoperative day 3 the patient was dischargedto home with improved symptoms. No pancreatic leak was detected and his insulin level return to normal [6,8mu/l]and blood glucose level was stabilized.
The pathology report confirmed the diagnosis of insulinoma.
Case 2:
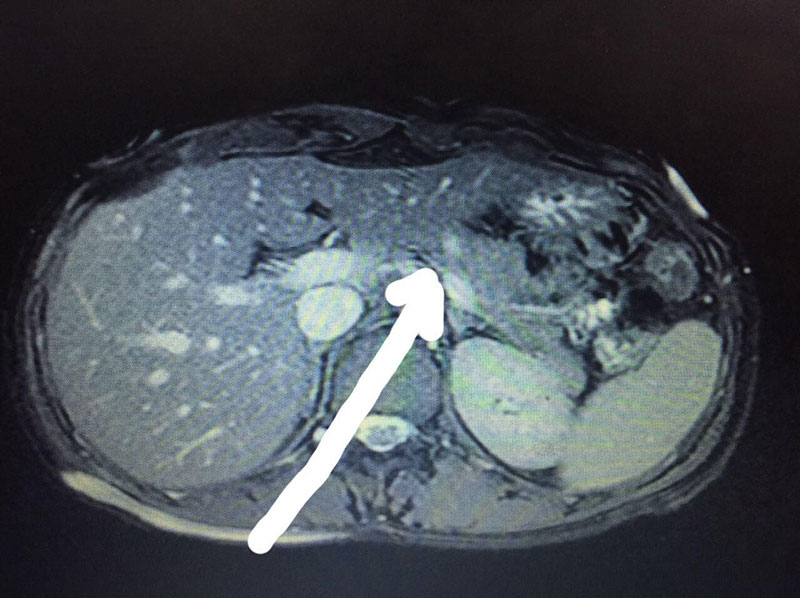
30 years old female presented with syncopal attacks with recurrent drops in her blood glucose levels below 50 mg/dl. Her insulin level was 288mu/l with elevated c-peptide level. Other biochemical investigations regarding adrenal gland were within normal value. CT scan of the abdomen with IV contrast reveals 7 mm enhancing nodule at the middle of pancreatic body. EUS revealed small suspicious nodule seen at the proximal pancreatic body. The nodule size was 6?6 mm. MRI with iv contrast found 7 mm high S1 nodule on T2 located at the pancreatic body directly under peritoneal cover.
MRI .IV contrast show small pancreatic mass case 2
The patient was admitted 48 hours before surgery with hypertonic glucose infusion and glucose monitoring every 4 hours. 8 hours before surgery the patient was put on nill per os.
The operation was done under general anasthesia, supine position, 4 port-incision, we opened the lesser sac, retracted the stomach upwards, dissected the pancreatic mass, and enucleated the mass. We put a drain in the laser sac. The operation was uneventful. The operating time was 75 minutes. The patient was discharged day 2 postoperative with improvement in her symptoms and stabilization of her insulin level (4.4mu/l) and blood glucose level. There was no postoperative pancreatic leak.
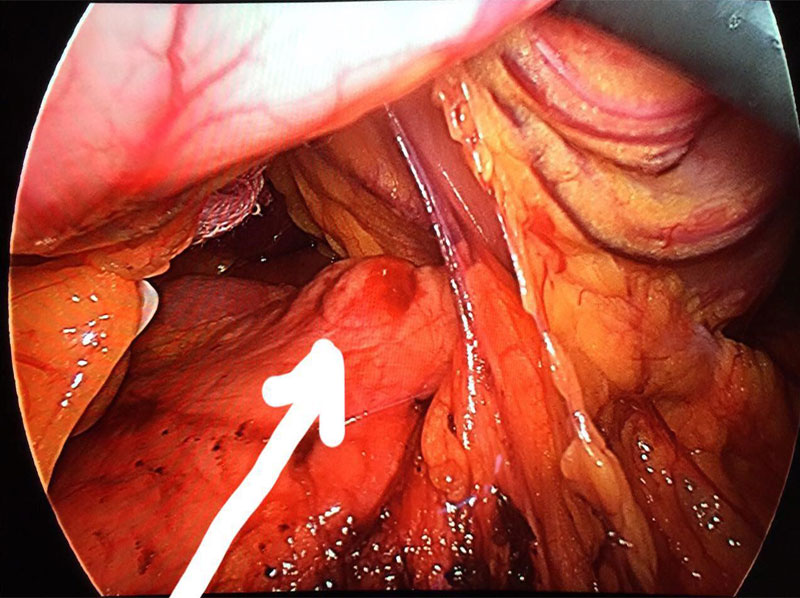
This is panceatic mass under pertoneal cover case 2
This is pancreatic mass dissected from pertoneal cover case 2
The pathology report confirmed the diagnosis of Beta Islet hyperplasia.
Discussion
Laparoscopic localization and resection of insulinomas are feasible and safe.
Pancreatic insulinoma surgical treatment is usually done by either classical open resection, or, as we prefer, laparoscopic enucleation of the tumor.
It is essential to localize the tumor before surgery, and confirm it during the operation with intraoperative ultrasound, which has a high rate of detection of the insulinoma (83 – 100%) and is regarded as the most sensitive method available.
It is feasible to avoid damaging the surrounding tissue using the ligasure device, with adequate retraction and electric dissection.
It is important to avoid unnecessary large abdominal incision for a small mass that can be enucleated with laparoscopic technique, which is the main advantage of laparoscopic surgery. Other advantages include less postoperative pain and early discharge, early return to his job.