Laparoscopic cholecystectomy for Gallbladder carcinoma confined to the gallbladder (Nov. 2020)
Review of literature
Gallbladder carcinoma
Author: Ashwin S. Akki, M.D, Ph.D.
Deputy Editor-in-Chief: Raul S. Gonzalez, M.D.
Topic Completed: 21 April 2020
Minor changes: 22 April 2020
Copyright: 2003-2020, PathologyOutlines.com, Inc.
Definition / general
Carcinoma arising from the gallbladder epithelium (WHO Classification of Tumours Editorial Board: Digestive System Tumours (Medicine), 5th Edition, 2019)
Essential features
Aggressive cancer, with an overall 5 year survival rate of < 10%
Cholelithiasis is a major risk factor
Up to 50% are detected incidentally in routine cholecystectomy specimens due to absence of gross abnormalities; systematic sampling of these specimens is therefore crucial to detect incidental gallbladder adenocarcinomas (Am J Surg Pathol 2019;43:1668)
Terminology
Carcinoma of gallbladder; adenocarcinoma of gallbladder; malignant epithelial neoplasm of gallbladder
ICD coding
ICD 10:
C23 ? malignant neoplasm of gallbladder
ICD-0:
8140/3 ? adenocarcinoma NOS
8070/3 ? squamous cell carcinoma NOS
8020/3 ? carcinoma, undifferentiated, NOS
ICD 11:
2C13.z ? malignant neoplasms of gallbladder, unspecified
Epidemiology
Commonly occurs in the sixth and seventh decades
F:M = 3:1
Highest incidence in women from Chile (27.3/100 000), India (21.5/100 000), Pakistan (13.8/100 000) and Ecuador (12.9/100 000) (Int J Cancer 2010;127:2446, Histopathology 2009;55:218)
Incidence 1.1 per 100,000 in the United States (Cancer Epidemiol Biomarkers Prev 2015;24:1319)
Overall 5 year survival rate of < 10%
Sites
Primarily affects the fundus (60%), body (30%) or neck (10%) of gallbladder
Advanced tumors involve the liver and extrahepatic biliary tree
Pathophysiology
Longstanding cholelithiasis and cholecystitis give rise to metaplastic changes (intestinal or pseudopyloric types) in the gallbladder mucosa (Cancer 1993;72:1878)
Metaplasia (especially intestinal type) gives rise to epithelial dysplasia and carcinoma in situ (J Hepatobiliary Pancreat Surg 2000;7:556)
Progression from dysplasia to advanced gallbladder carcinoma takes around 15 years (Gastroenterology 1996;111:232)
Etiology
Risk factors include:
Cholelithiasis (major risk factor)
Chronic cholecystitis, especially hyalinizing cholecystitis
Obesity
Infections (esp. Salmonella and Opisthorchis viverrini)
Porcelain gallbladder
Primary sclerosing cholangitis
Pancreaticobiliary maljunction (supra-Oddi union of common bile duct with the main pancreatic duct)
Occasionally occurs in patients with Lynch syndrome or familial adenomatous polyposis (FAP)
Clinical features
Asymptomatic in a large majority of patients
Symptoms when present are vague
Right upper quadrant pain (most common)
Weight loss
Fever
Disease is usually advanced by the time patient develops symptoms
Diagnosis
50% are diagnosed incidentally on routine cholecystectomy specimens
Finding a thickened gallbladder wall or polypoid lesions in the gallbladder on imaging done for other reasons should prompt surgical resection
Laboratory
Elevated alkaline phosphatase in advanced cancers (HPB (Oxford) 2008;10:446)
CEA only has 50% sensitivity (Int J Cancer 1990;45:821)
Radiology description
Imaging findings are variable from subtle (in early disease) to obvious (in late disease)
Thickening of the gallbladder wall
Raised / polypoid lesion in the gallbladder wall / lumen
Mass occupying or replacing the gallbladder lumen
Gallbladder mass invading the liver (in advanced disease)
Ultrasound is the primary imaging modality for screening purposes in suspected cases
Abnormal findings on ultrasound are further investigated by CT and MRI that provide detailed information, including staging parameters\
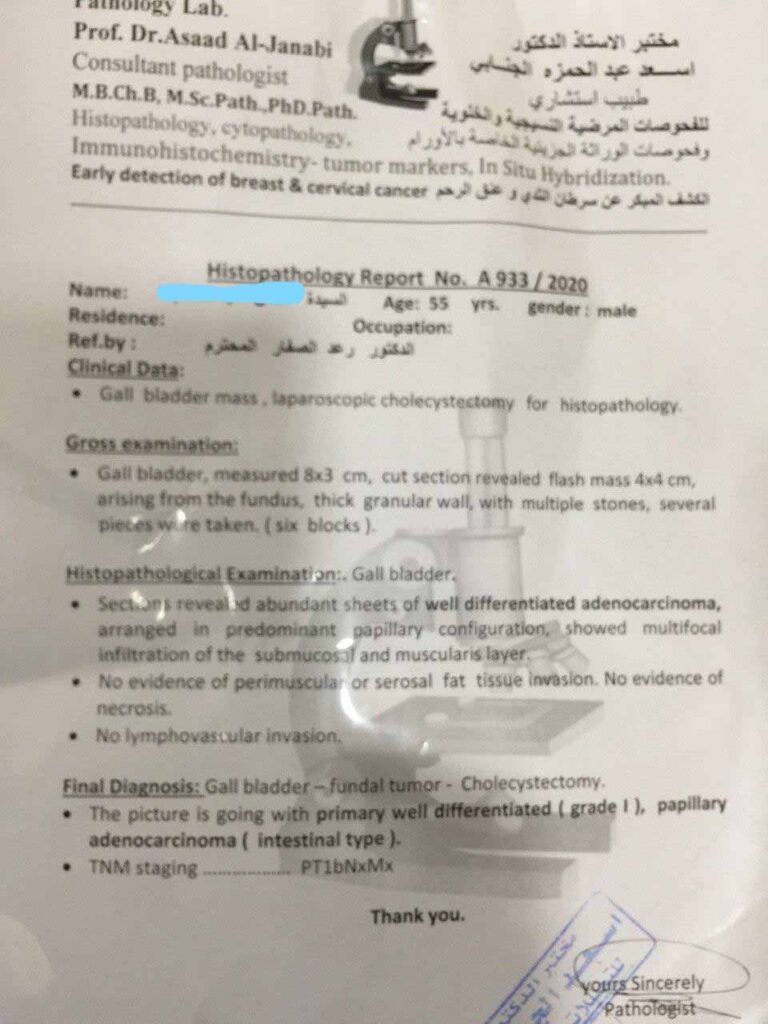
Prognostic factors
Noninvasive papillary carcinomas, regardless of size and differentiation, do not metastasize
Invasive papillary carcinomas have the most favorable prognosis (Arch Pathol Lab Med 2005;129:905)
Prognosis of adenocarcinoma, NOS depends on tumor stage:
Superficially invasive cancers limited to the lamina propria (pT1a) have excellent prognosis as they are completely cured by cholecystectomy (Ann Surg 2017;266:625)
Advanced cancers (i.e. muscle invasive and beyond; pT1b ? pT4) have a higher chance of recurrence and have poorer outcomes (J Gastrointest Surg 2007;11:631, Ann Surg 2011;254:320)
High histologic grade (poor differentiation) and vascular invasion have adverse outcomes (Cancer 1992;70:1493)
Rokitansky-Aschoff sinus involvement by carcinoma and cystic duct margin status are suspected predictors of progression (Am J Clin Pathol 2014;141:675)
Case reports
22 year old man with primary signet ring cell carcinoma of gallbladder in the absence of choleliths (Int J Surg Pathol 2010;18:358)
56 year old woman with clear cell carcinoma of the gallbladder (Int J Surg Case Rep 2017;32:36)
59 year old woman with hepatoid carcinoma of the gallbladder (World J Surg Oncol 2011;9:103)
62 year old man with carcinosarcoma of the gallbladder with chondroid differentiation (Int J Clin Exp Pathol 2015;8:7464)
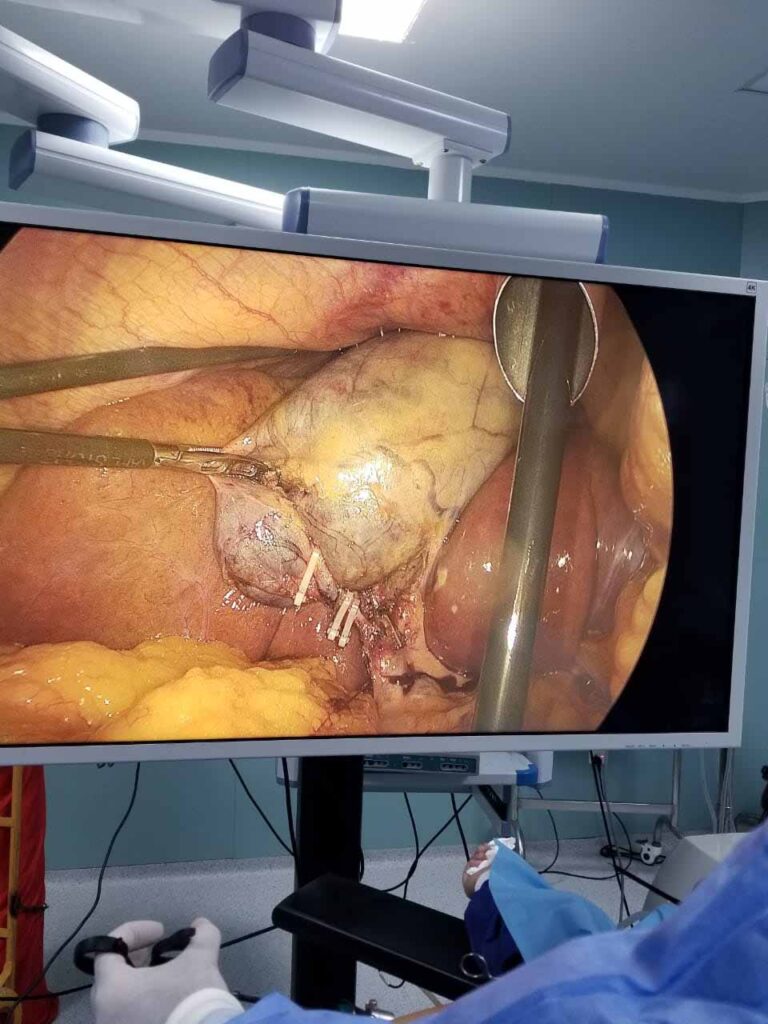
Treatment
Cholecystectomy with a negative cystic duct margin is curative in pT1a tumors (Ann Surg 2017;266:625)
Hilar / portal lymphadenectomy, plus resection of hepatic bed and the common bile duct to achieve negative margins, is necessary for tumors that extend into a muscle or beyond (pT1b ? pT3) (HPB (Oxford) 2015;17:681)
Chemotherapy or radiation for metastatic tumors
Gross description
Incidental gallbladder cancer in routine cholecystectomy specimens can be grossly subtle, with areas of mucosal granularity / irregularity, minimally raised / polypoid mucosal lesions or focally thickened fundus / body (Am J Surg Pathol 2019;43:1668)
Frank tumors may have one or more of the following features:
Thickened and indurated gallbladder wall
Exophytic or polypoid friable mucosal lesions (especially those arising from intracholecystic papillary neoplasm)
Firm, gritty, tan-white to yellow-gray cut surface.