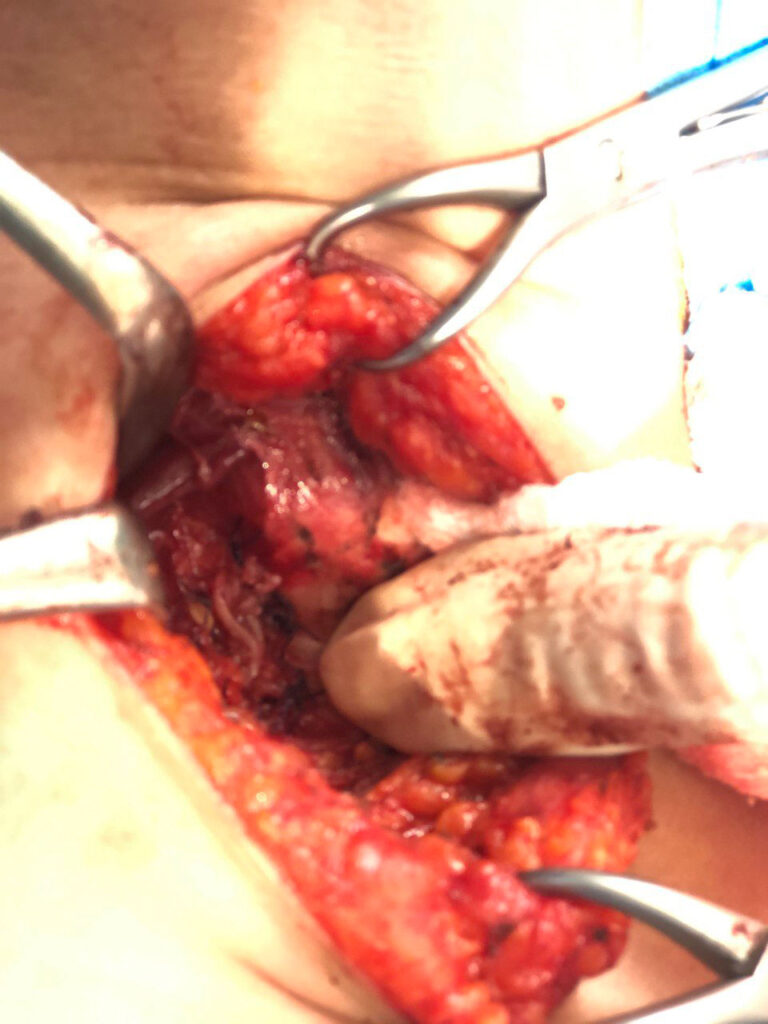
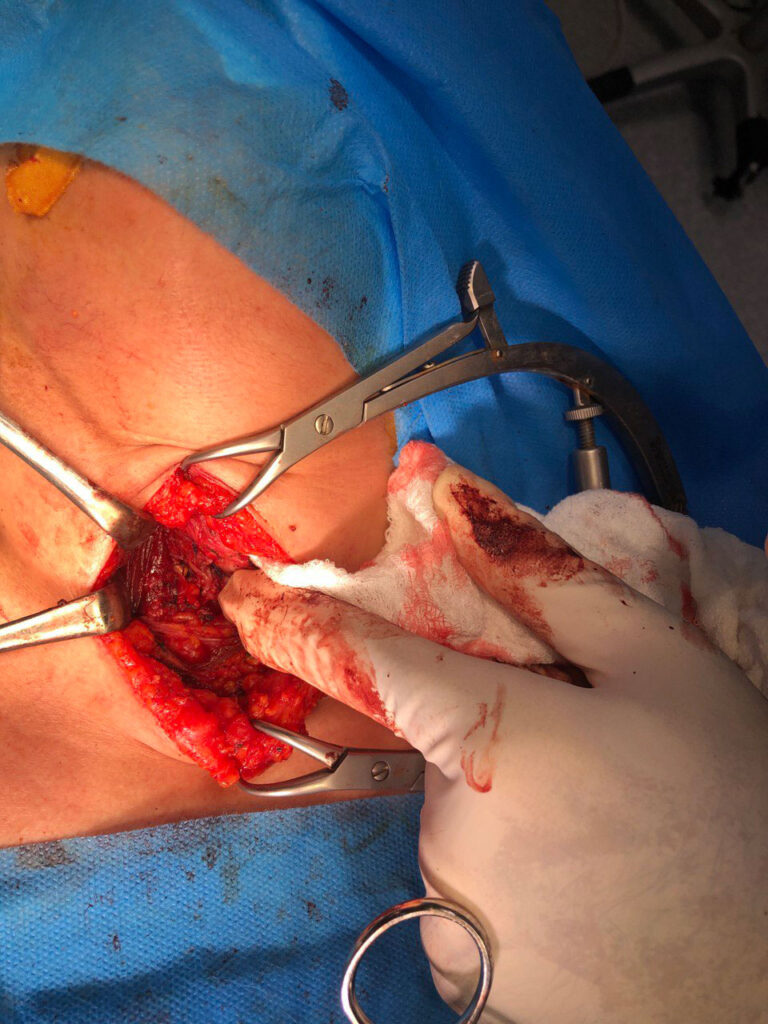
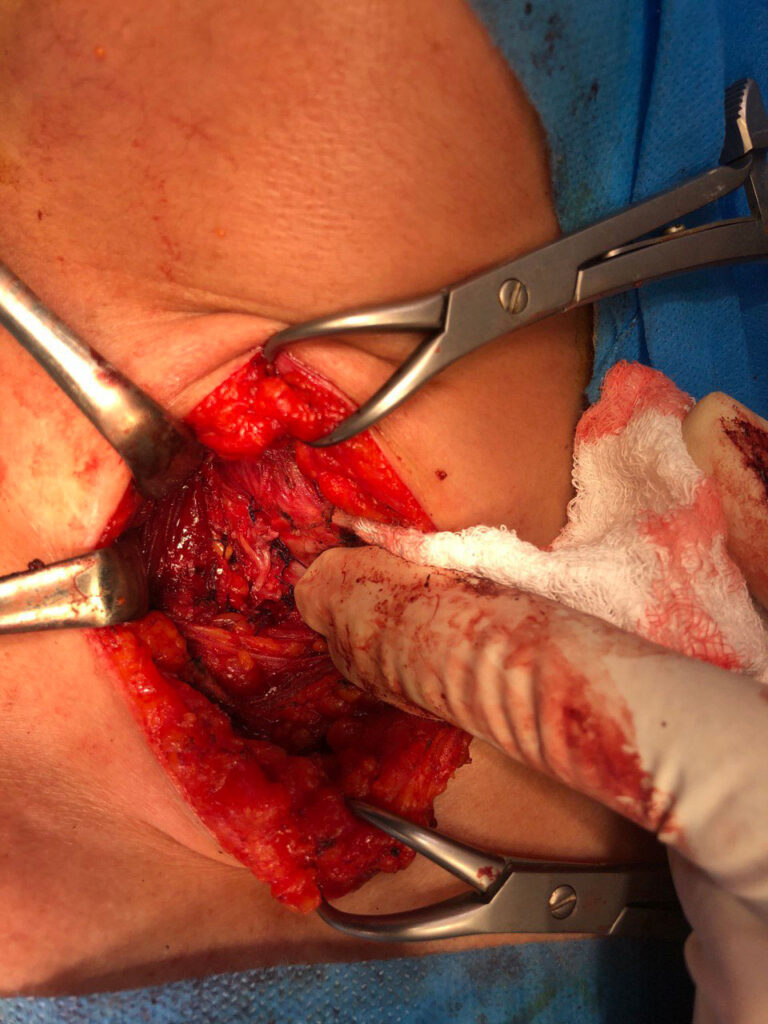
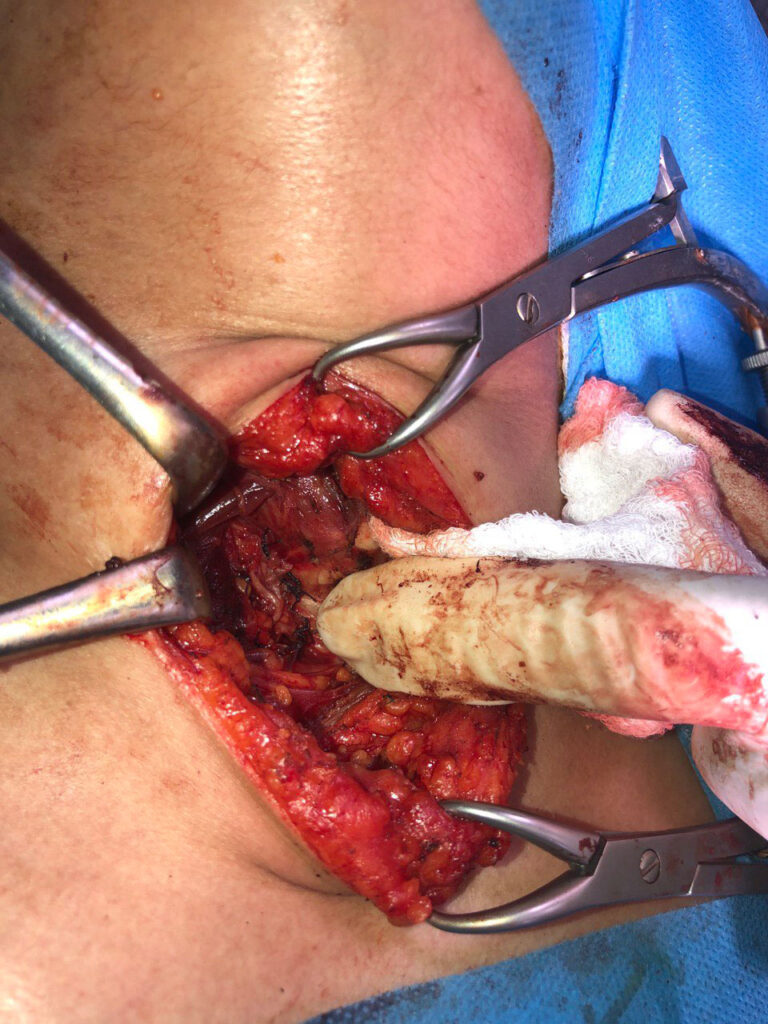
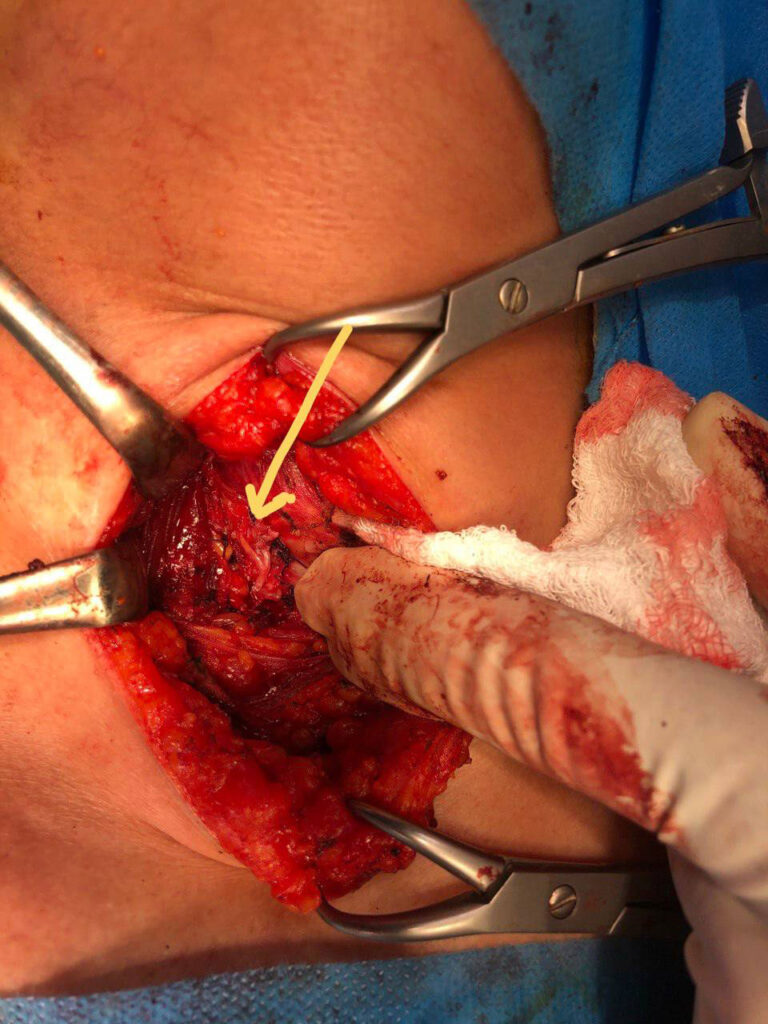
BRANCHING RLN finding during total thyroidectomy (June.2022)
Review of literature
Extralaryngeal branching of the recurrent laryngeal nerve: a meta-analysis of 28,387 nerves
Brandon Michael Henry, Jens Vikse, […], and Krzysztof A. Tomaszewski
Abstract
Introduction
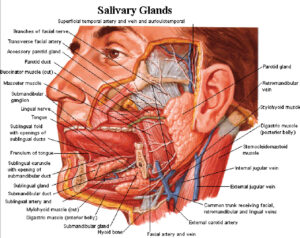
The recurrent laryngeal nerves (RLN) are branches of the vagus nerve that go on to innervate most of the intrinsic muscles of the larynx. Historically, the RLN has been considered to branch after it enters the larynx, but numerous studies have demonstrated that it often branches before. The wide variability of this extralaryngeal branching (ELB) has significant implications for the risk of iatrogenic injury. We aimed to assess the anatomical characteristics of ELB comprehensively.
Methods
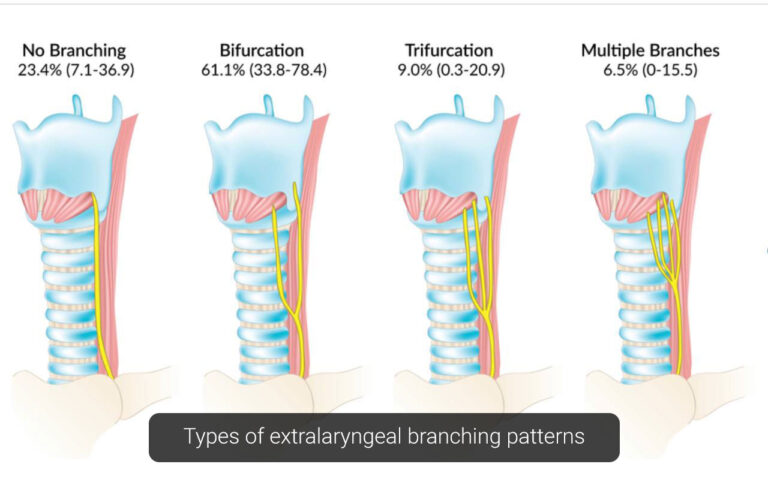
Articles on the ELB of the RLN were identified by a comprehensive database search. Relevant data were extracted and pooled into a meta-analysis of the prevalence of branching, branching pattern, distance of ELB point from the larynx, and presence of positive motor signals in anterior and posterior ELB branches.
Results
A total of 69 articles (n = 28,387 nerves) from both intraoperative and cadaveric modalities were included in the meta-analysis. The overall pooled prevalence of ELB was 60.0 % (95 % CI 52.0–67.7). Cadaveric and intraoperative subgroups differed with prevalence rates of 73.3 % (95 % CI 61.0–84.0) and 39.2 % (95 % CI 29.0–49.9), respectively. Cadavers most often presented with a ELB pattern of bifurcation, with a prevalence of 61.1 %, followed by no branching at 23.4 %. Branching of the RLN occurred most often at a distance of 1–2 cm (74.8 % of cases) prior to entering the larynx. A positive motor signal was most often noted in anterior RLN branches (99.9 %) but only in 1.5 % of posterior branches.
Conclusions
The anatomy of the RLN is highly variable, and ELB is likely to have been underreported in intraoperative studies. Because of its high likelihood, the possibility of ELB needs to be assessed in patients to prevent iatrogenic injury and long-term postoperative complications.