Brunner’s galnd hamartoma (Dec. 2017)
Case report
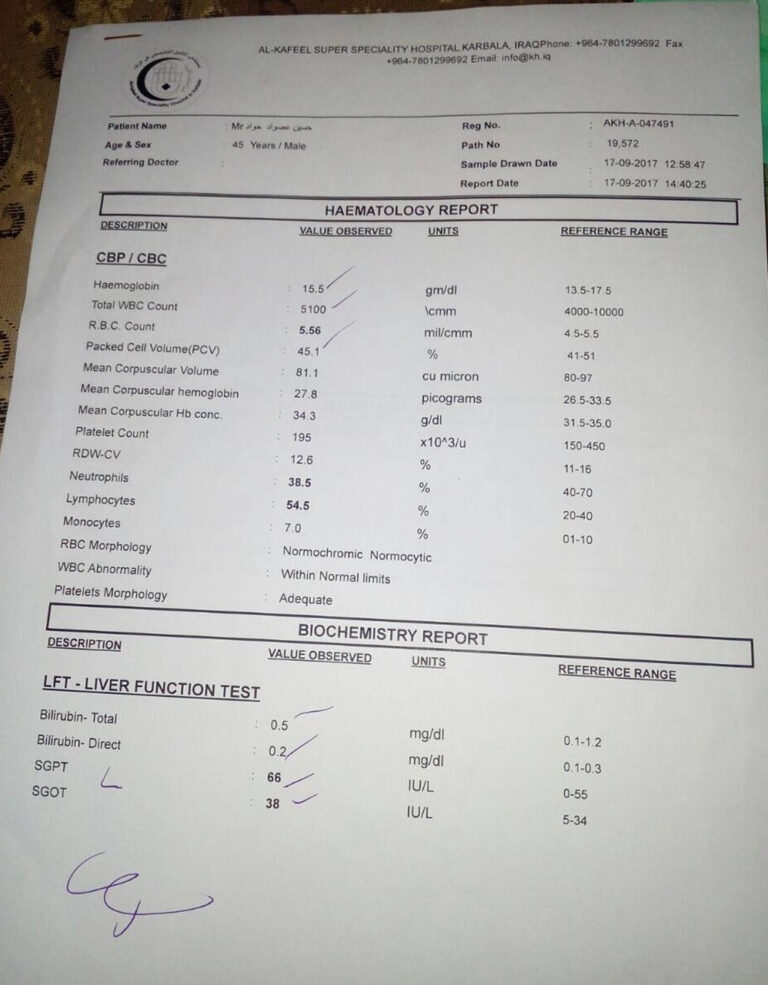
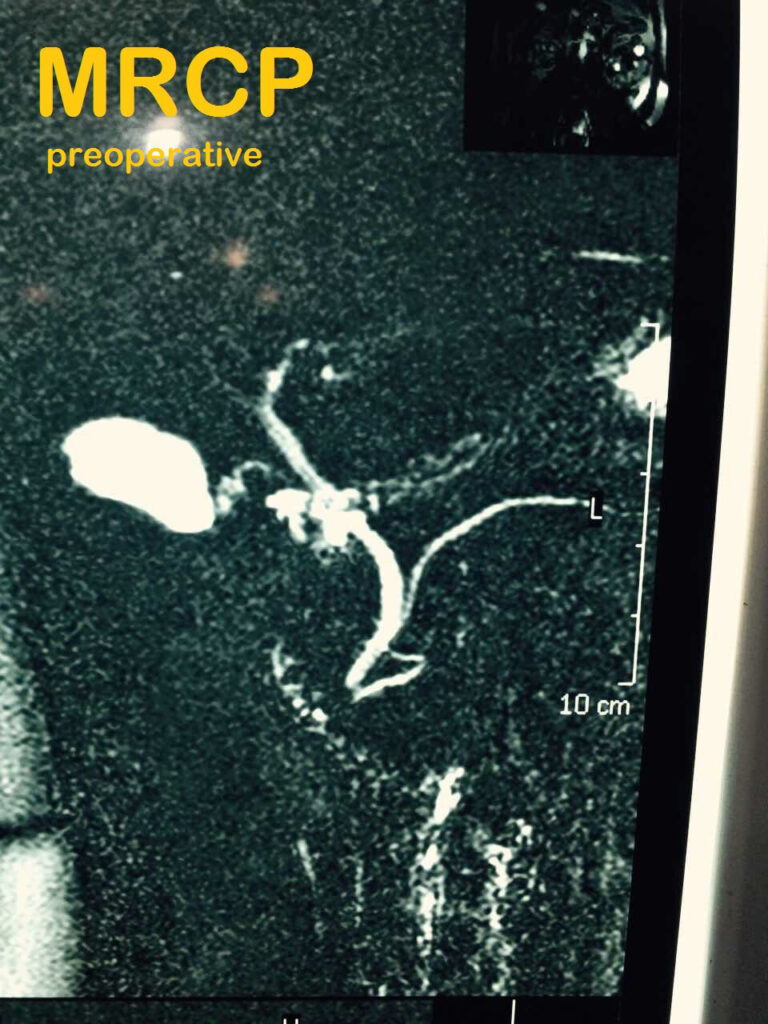
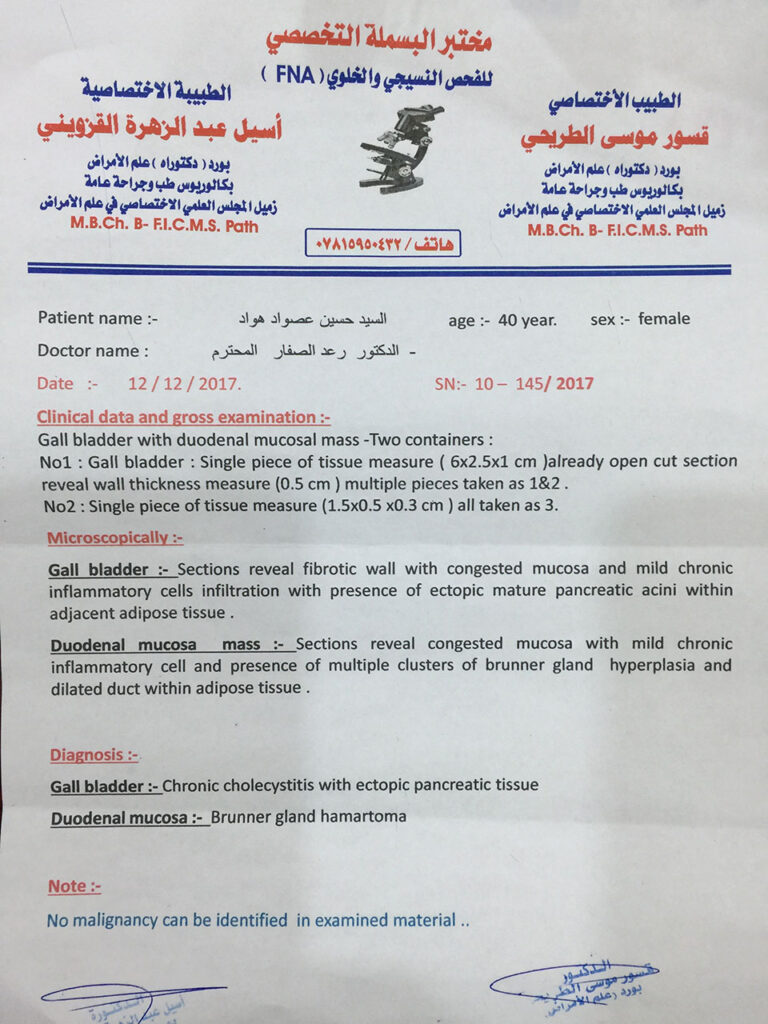
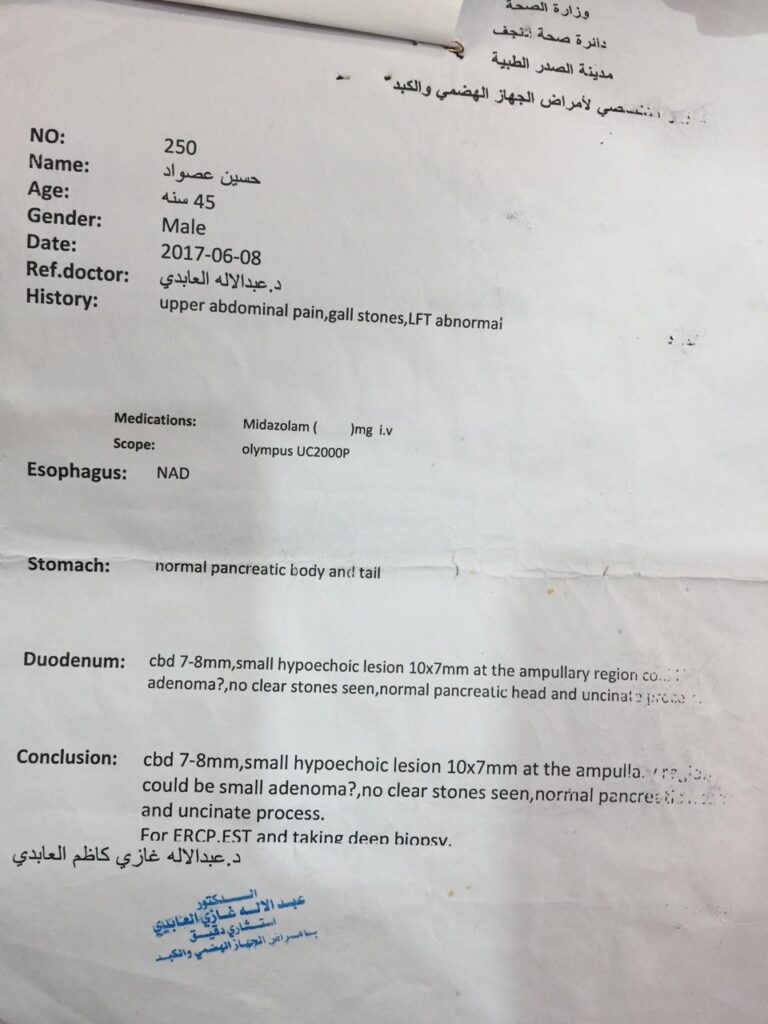
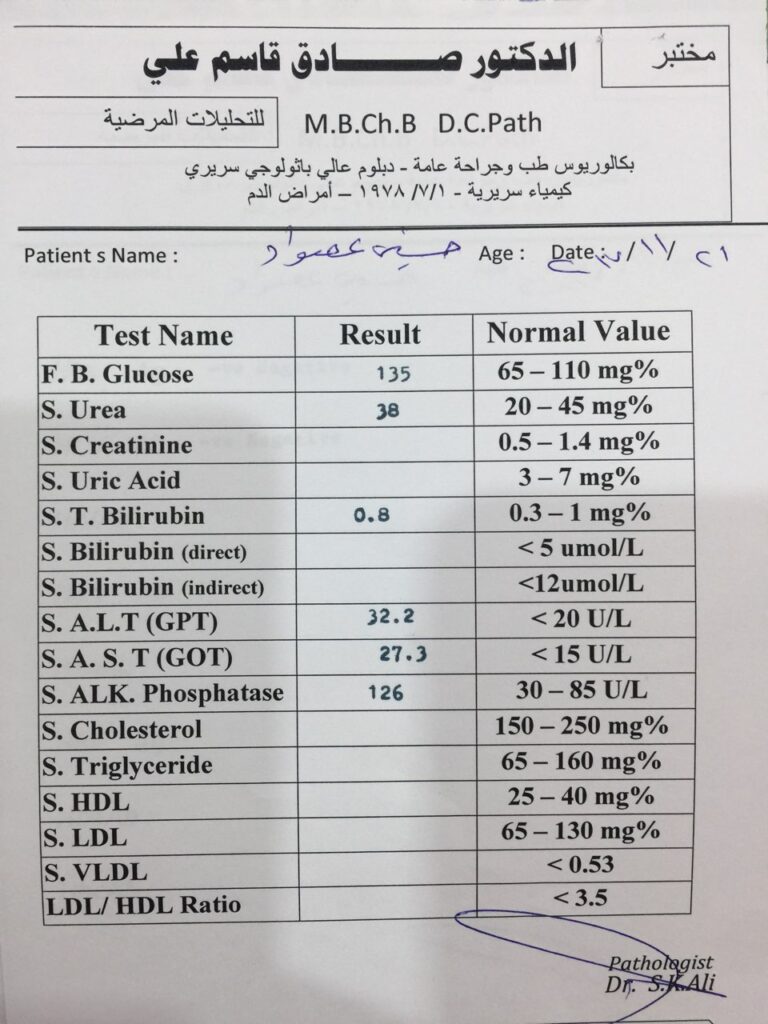
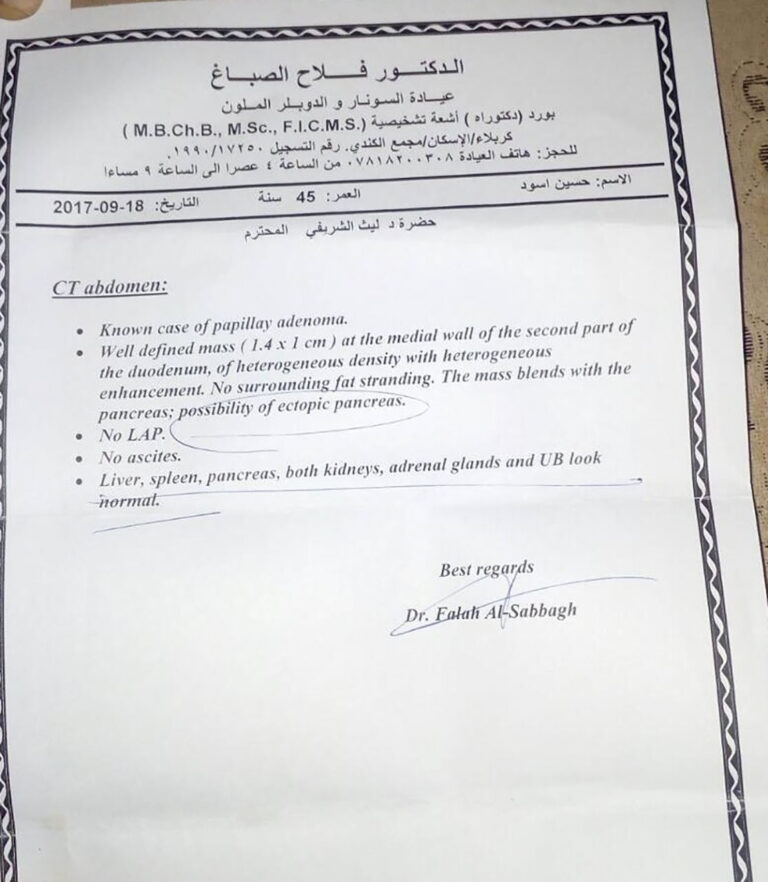
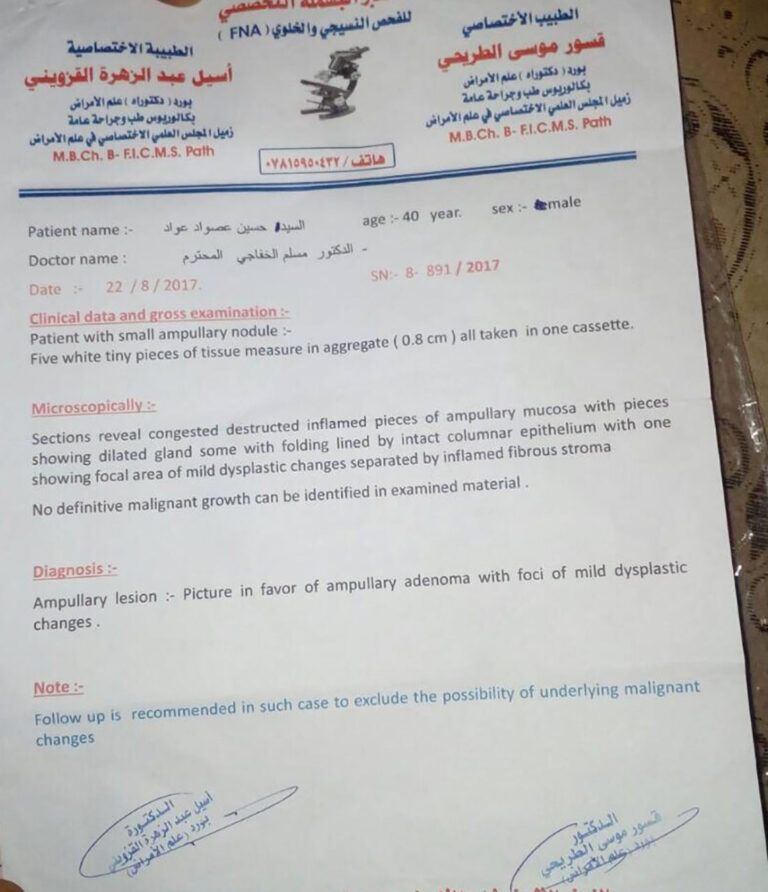
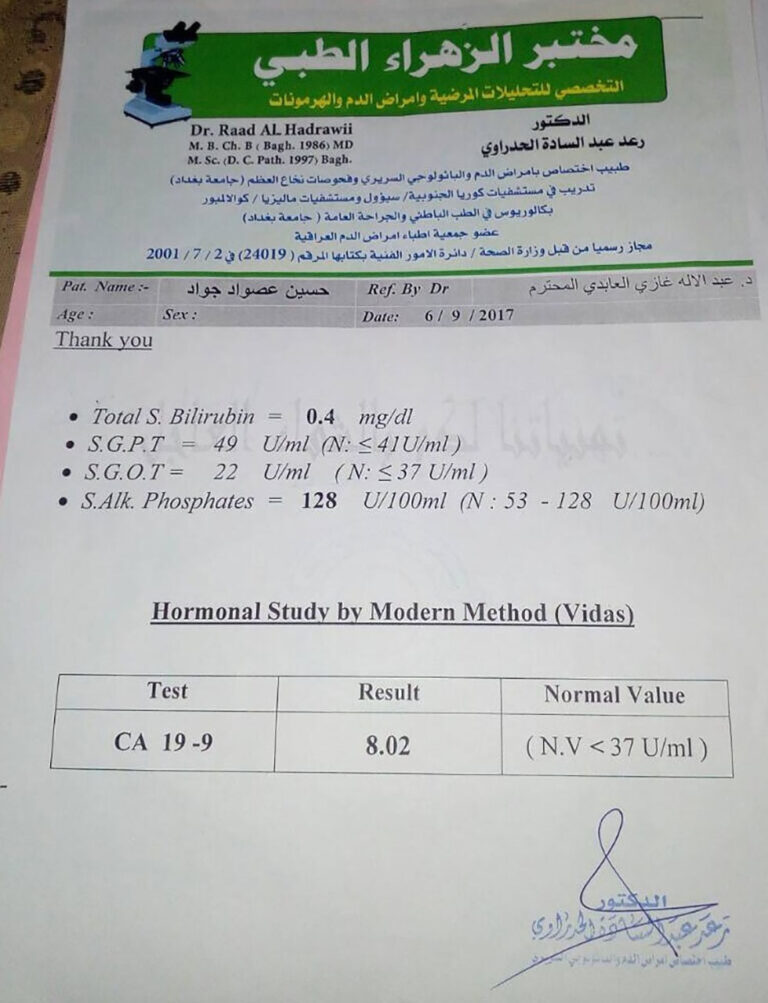
40 years old male patient presented with recurrent attacks of biliary colic and mild jaundice in 3 months period. Abdominal examination and abdominal ultrasound were unremarkable. Abdominal CT SCAN revealed small duodenal mass 1.4 * 1 cm
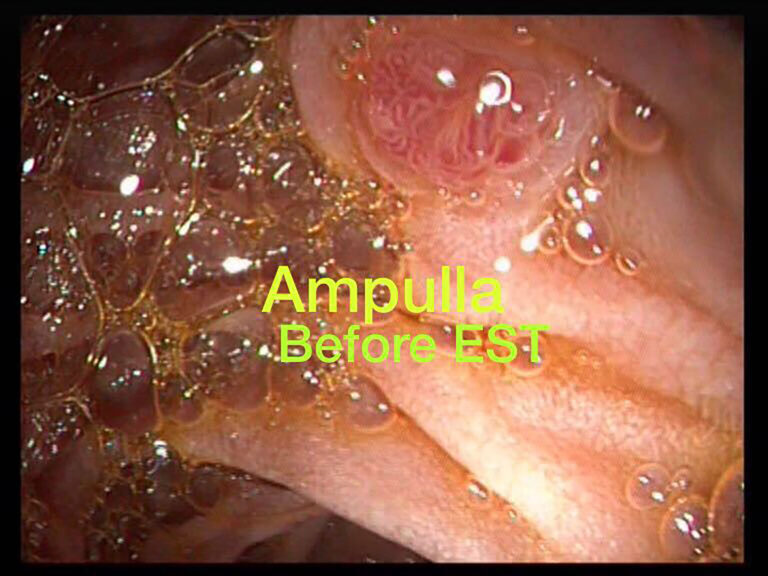
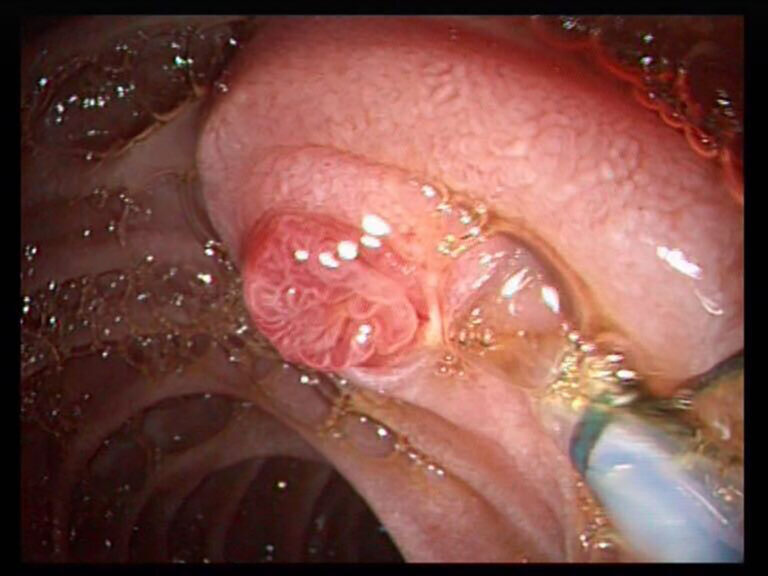
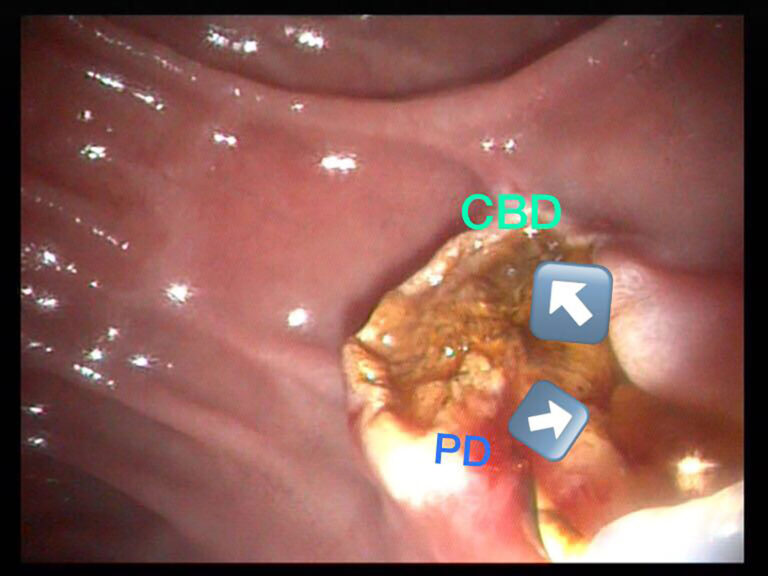
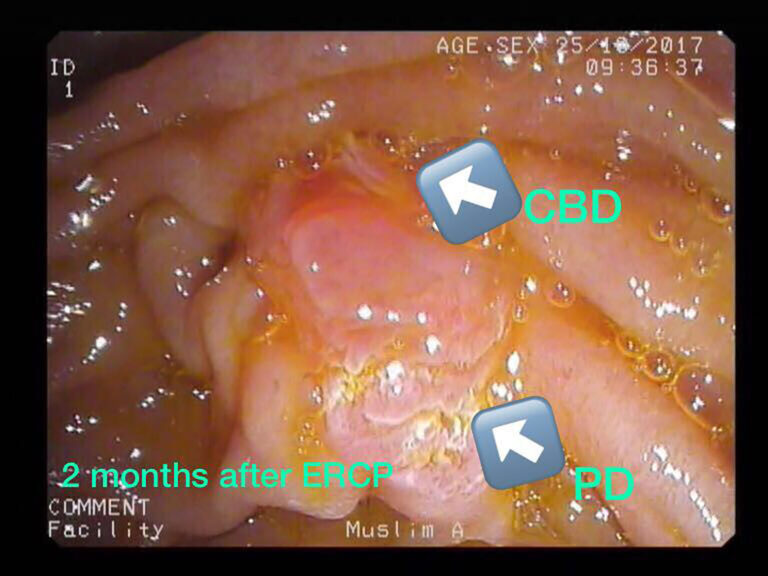
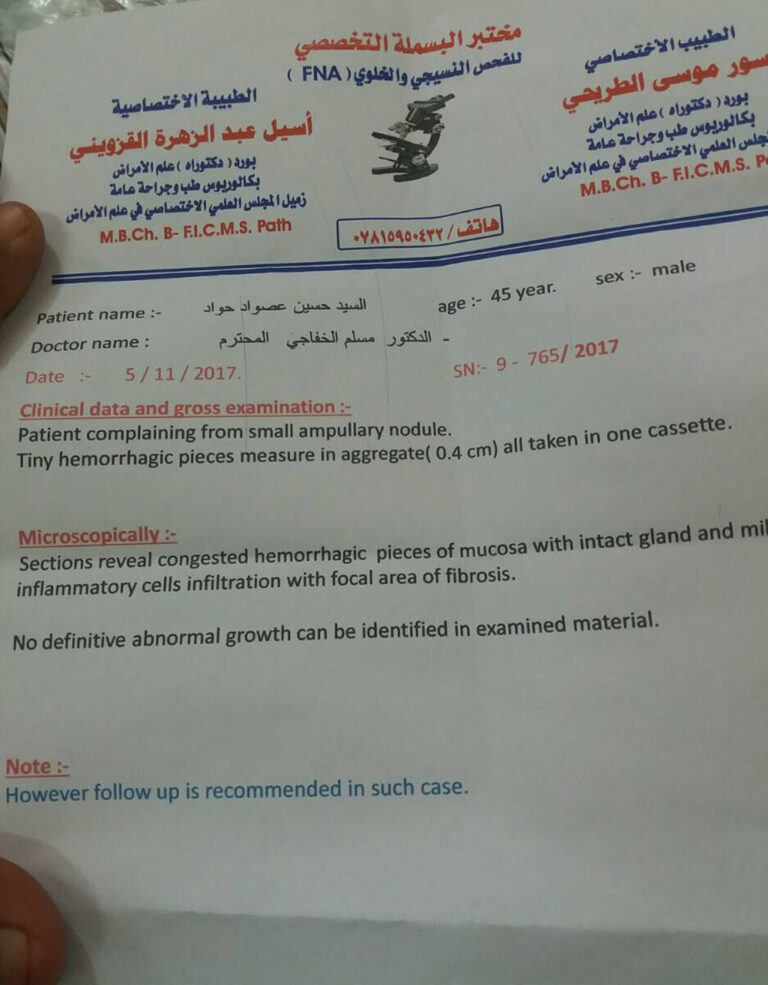
Upper endoscopy and EUS were done and revealed mild CBD dilation with sludge plus duodenal nodule near the ampulla. ERCP was done to the patient and biopsy with sphincterotomy were achieved. Histopathological examination result was ampullary adenoma
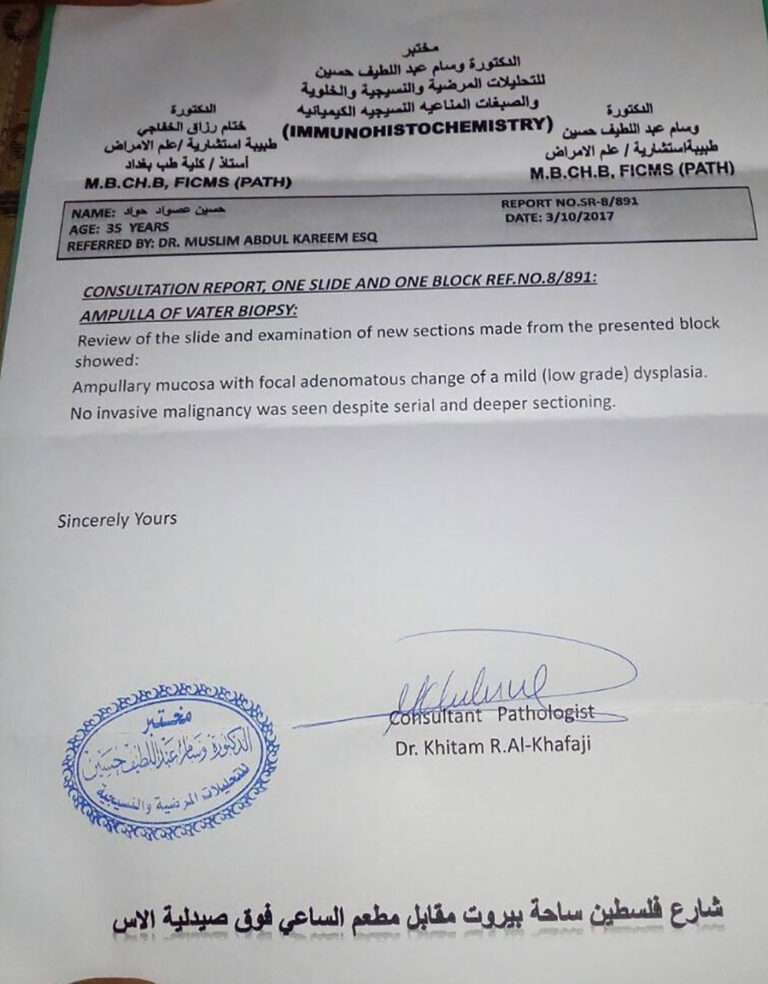
The patient got little improvement and duodenoscopy repeated after 2 months and another biopsy taken from same nodule and histopathology revealed adenoma with mild dysplasia. The patient was arranged for ampullectomy operation.
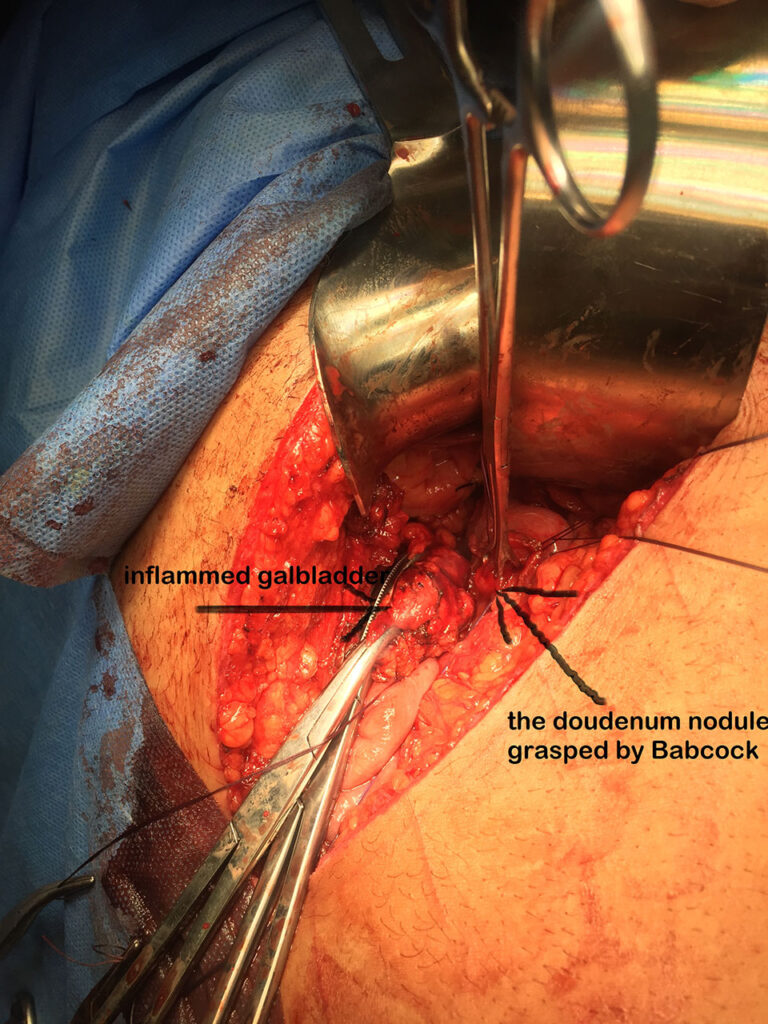
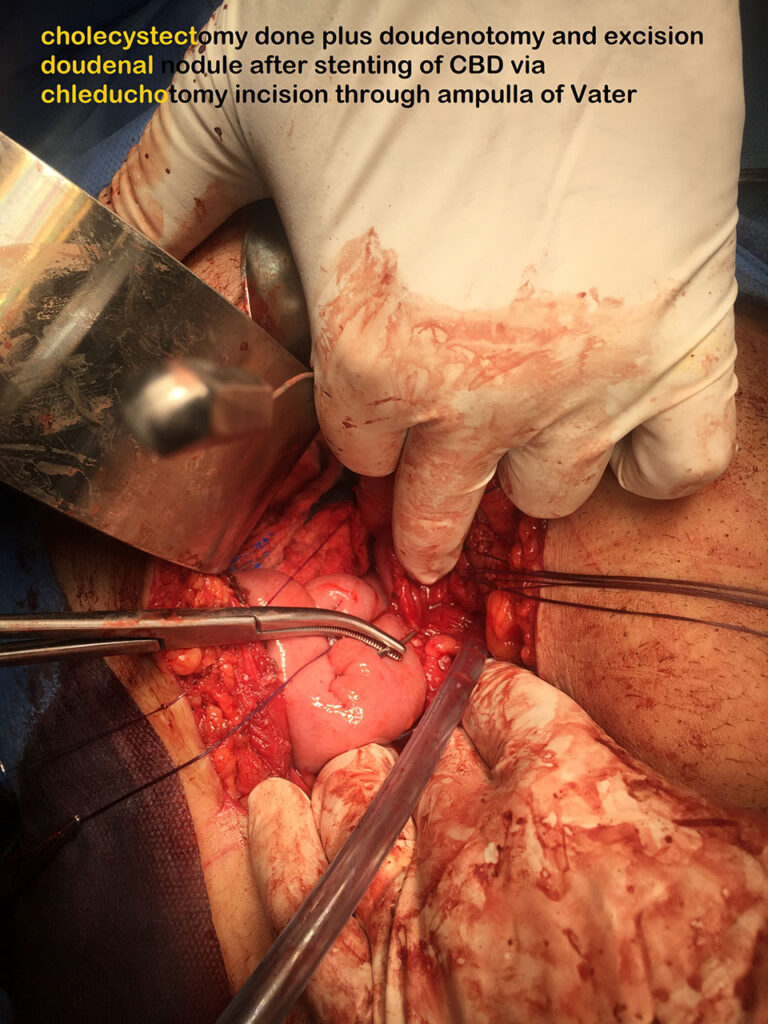
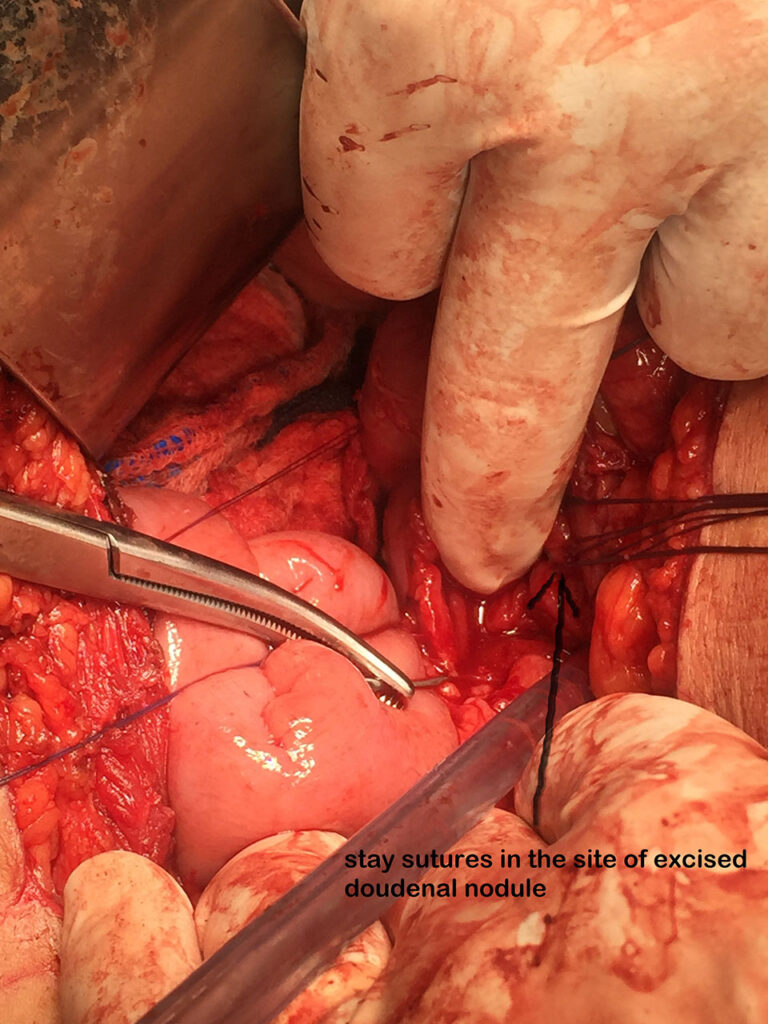
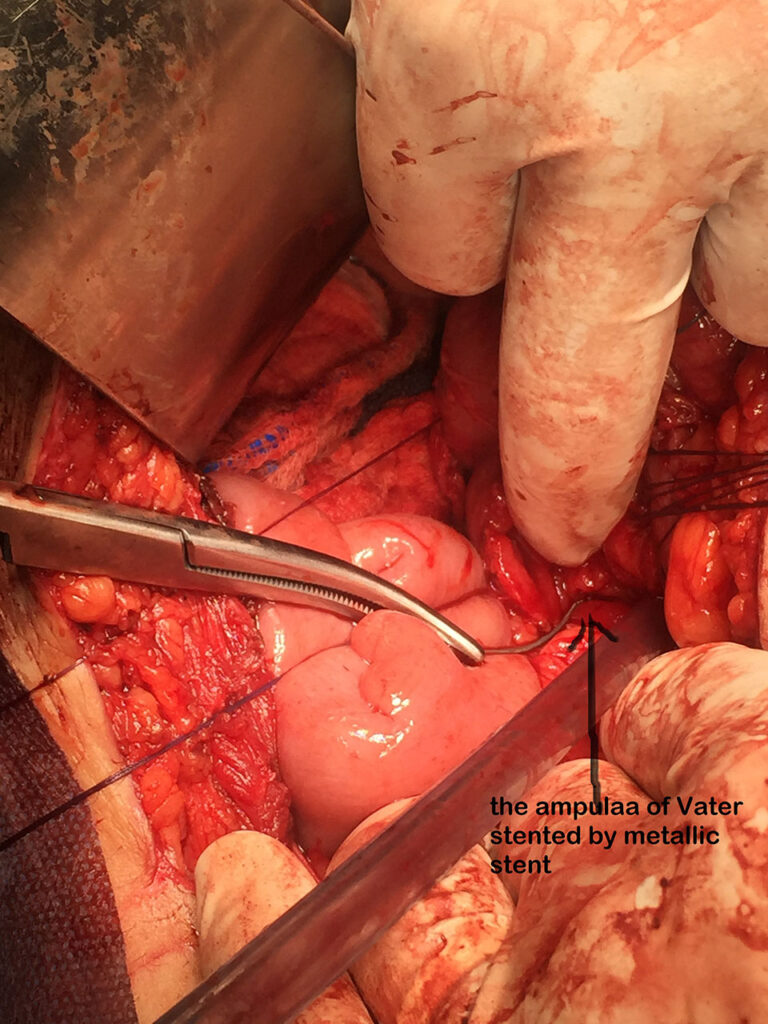
Operative findings were thick wall gallbladder and intraluminal palpable duodenal nodule. Cholecystectomy and choleduchotomy were done plus duodenotomy. The duodenal nodule less than 2 cm was found away from the ampulla. The ampulla stented by metallic stent via choleduchotomy and the nodule excised and duodenotomy closed. T – tube was inserted in CBD and intraabdominal drain put in Morrison’s pouch Laparotomy subcostal incision closed in layers The postoperative course was uneventful.
Histopathology report revealed 2 rare findings:
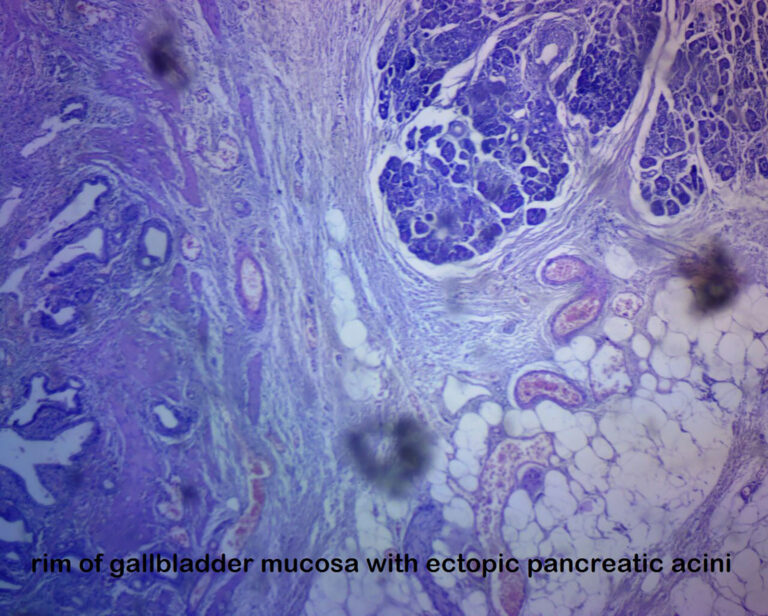
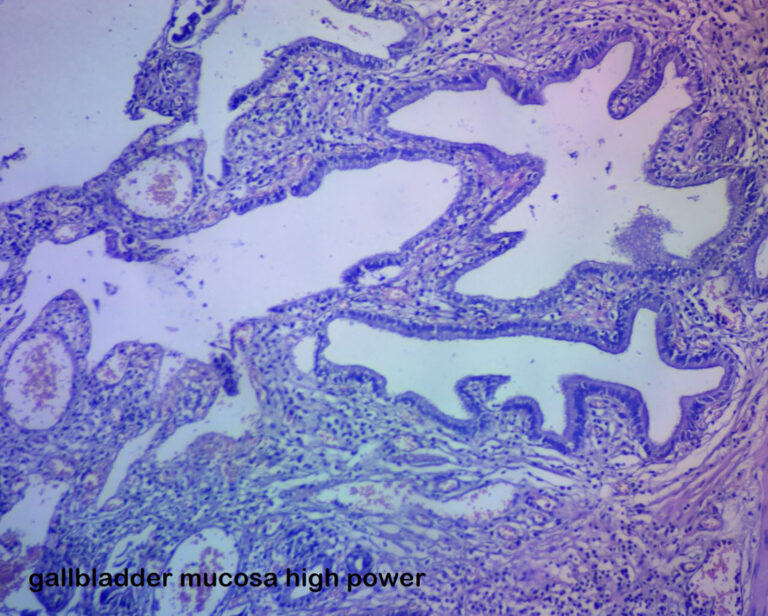
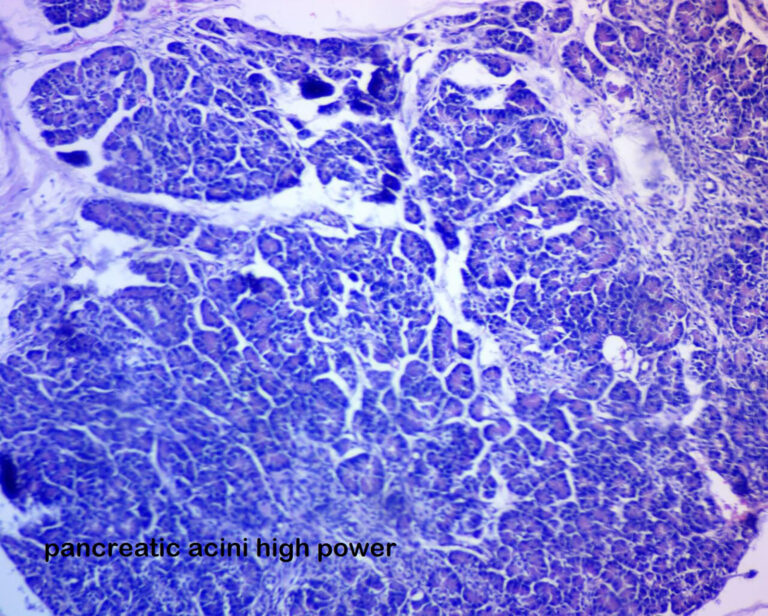
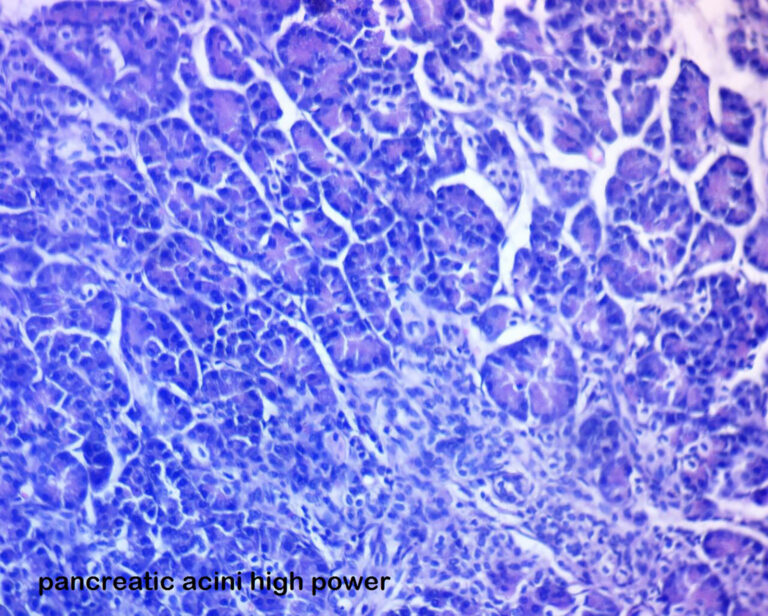
- ectopic pancreatic tissue in the gallbladder
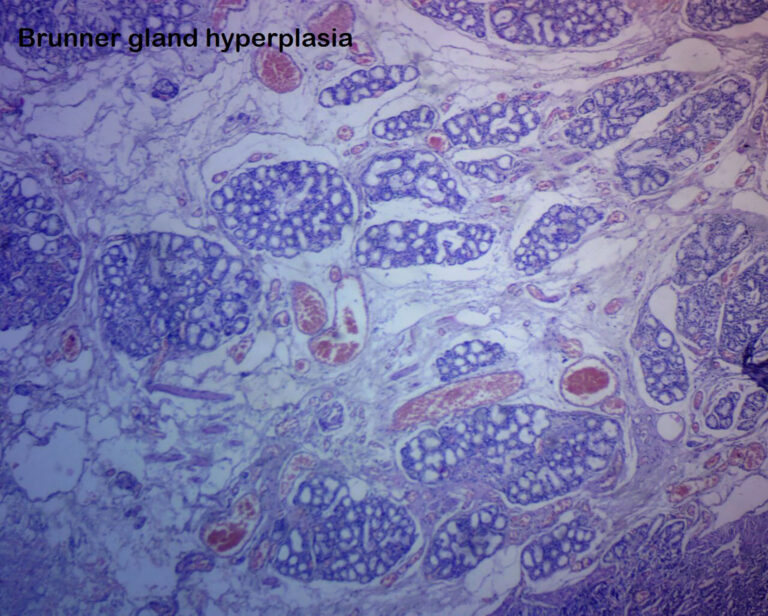
- duodenal nodule was Brunner’s gland hamartoma.
- Ann R Coll Surg Engl. 2015 Jul; 97(5): e70–e72.
- Published online 2015 Jul. doi: 10.1308/003588415X14181254790040
- PMCID: PMC5096579
- Brunner’s gland hamartoma of the duodenum
- J Sedano, R Swamy, K Jain, and S Gupta
DISCUSSION
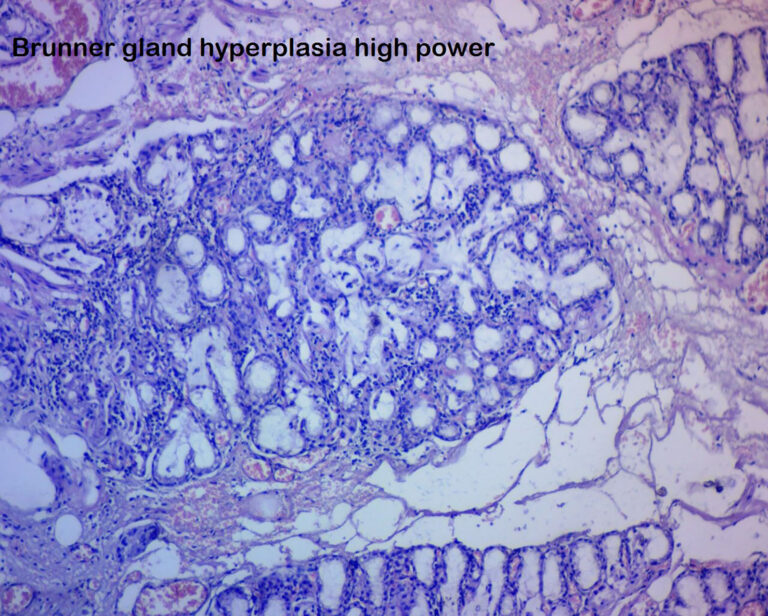
Also referred to as Brunner’s gland adenoma or Brunneroma, BGH is a rare benign tumour of the duodenum, featuring a proliferation of Brunner’s glands in the submucosa. They represent about 5–10% of benign duodenal tumours1 and have an estimated incidence of less than 0.01%.2 Hamartoma designates an excessive focal overgrowth of mature normal cells and tissues in an organ, composed of identical cellular elements. The term ‘Brunner’s gland hamartoma’ is favoured over ‘Brunner’s gland adenoma’ as they show an admixture of normal tissues including Brunner’s glands and ducts histologically. Adipose tissue, Paneth cells, mucus glands, pancreatic acini and lymphoid tissue usually without cellular atypia can also occur in BGH.1,2
Brunner’s glands are located in the submucosa of the duodenum. They secrete an alkaline fluid containing mucin, which protects the mucosa from the acidic stomach contents entering the duodenum.3 BGHs consist of an abnormal proliferation of Brunner’s glands, along with a mixture of adipose tissue, fibrous septa, smooth muscle and other normal tissue components.4 They present typically as a single polypoid and pedunculated mass with a normal mucosal surface. The distribution of BGHs in the small bowel reflects that of Brunner’s glands, with about 70% occurring in the proximal duodenum and a decreasing frequency occurring throughout the rest of the duodenum.4
The aetiology of BGH is unclear although it is suggested that hyperacidity or Helicobacter pylori may provoke proliferation of these protective glands.5 In addition to alkaline mucus, Brunner’s glands secrete urogastrone, which inhibits gastric acid secretion, and may have a protective role against peptic ulcer development. In a large study of 19,000 people, 5 out of 7 patients who were diagnosed with BGH were also found to have H pylori infection.6 However, the significance of this is unclear as the presence of H pylori is so commonplace.
BGHs are often asymptomatic and may be an incidental finding during endoscopy or imaging.7 BGHs may present acutely with gastrointestinal bleeding, bowel obstruction, or more insidiously with symptoms such as dyspepsia or anaemia.7,9 A study of 27 cases of BGH found that 37% presented with haemorrhage, 37% with bowel obstruction and the rest were incidental findings.4 In more unusual cases, BGH has led to intussuseption,3 obstructive jaundice and pancreatitis.9
Removal of a BGH is usually by endoscopic resection unless it is particularly large or broad-based, as in the present case. There have been reported cases where malignancy was suspected so a more radical procedure such as a pancreaticoduodenectomy was performed to ensure wide enough clear margins.10 In many cases, the histological diagnosis of BGH can only be confirmed after complete resection of the polyp as biopsies obtained during endoscopy may not be deep enough to demonstrate the glandular proliferation in the submucosal tissues.
BGHs are considered to be entirely benign tumours although there have been anecdotal reports of malignant foci in them.11 There are no reported recurrences following removal of a BGH and the long-term prognosis is excellent.