GIANT JUVENILE BREAST FIBROADENOMA (Oct.2020)
Case presentation
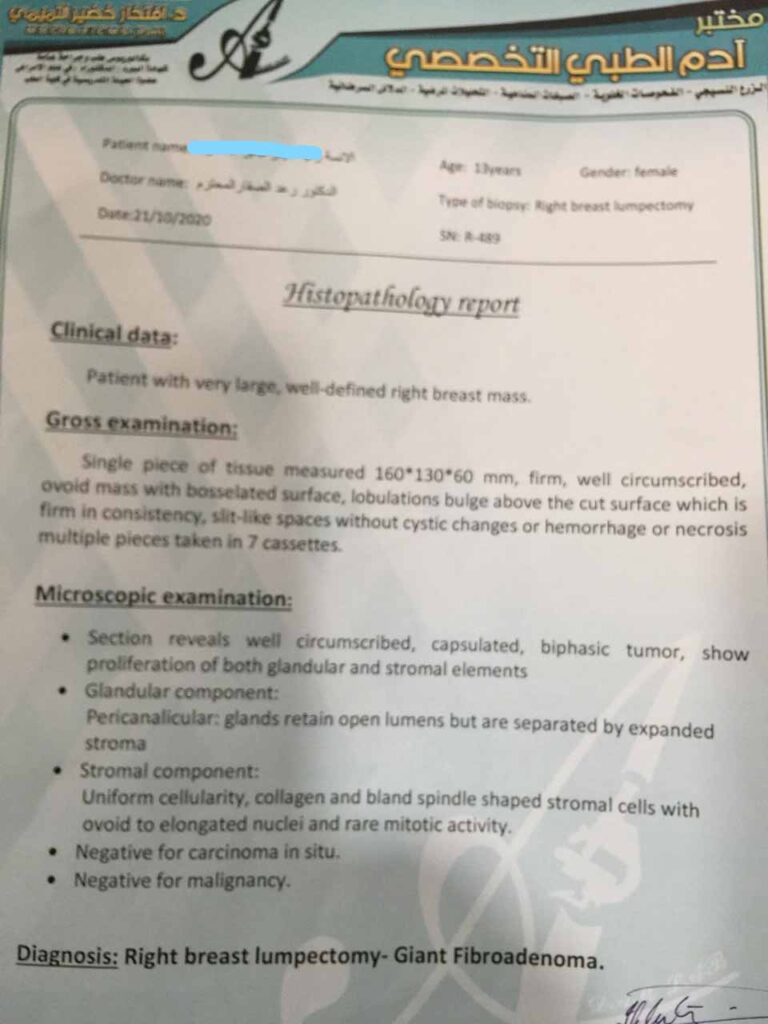
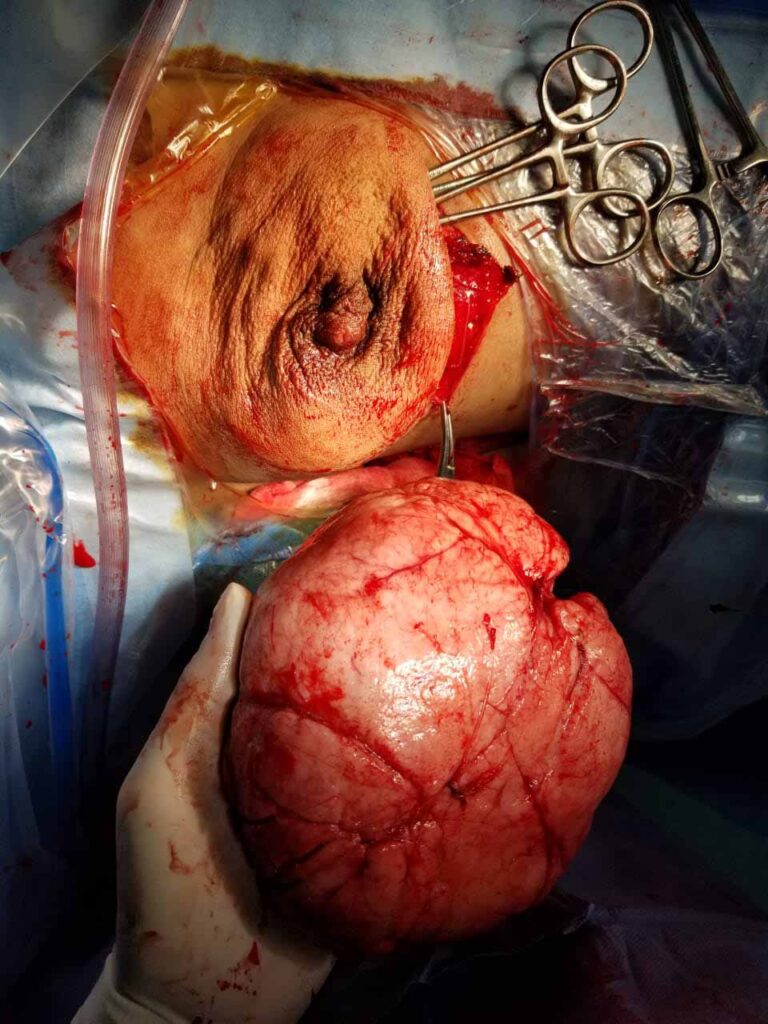
A 13-year-old female came to the surgical clinic with the chief complaints of asymmetrical breasts and a large lump in the right breast. She also complained of associated dragging non-radiating type of pain in the right breast since last 15 days. There was no history of breast trauma, fever, and anorexia or weight loss. Her past, medical and family history was non-contributory. On physical examination, the right breast was bigger than the left breast and the right nipple-areola complex was displaced inferiorly. On palpation, there was a lump in the right breast which measured 15×12 cm in size and was located in the right upper and lower inner quadrant . It was firm in consistency, non-tender, freely mobile within the breast tissue and free from the chest wall. The overlying skin was tense and shiny with prominent distended superficial veins. There was no skin ulceration or any nipple discharge. Her systemic examination, the left breast and bilateral axilla were within normal limits. Based on the patient’s age, history and the breast examination, a clinical diagnosis of giant fibro adenoma was made. Her routine hematological, biochemical and microbiological parameters were within normal limits.
Complete surgical excision was done through inframammary incision without need for reconstruction.
Review of literature
Giant juvenile fibroadenoma: a systematic review with diagnostic and treatment recommendations
Michael Sosin1,2, Marisa Pulcrano1, Elizabeth D. Feldman3, Ketan M. Patel4, Maurice Y. Nahabedian5, Jason M. Weissler6, Eduardo D. Rodriguez2
Department of Surgery, Medstar Georgetown University Hospital, Washington, DC, USA; 2Department of Plastic Surgery, Institute of Reconstructive Plastic Surgery, New York University Langone Medical Center, New York, NY, USA; 3Specialty Physicians of Northern Virginia, Reston Hospital Center, Reston, VA, USA; 4Department of Plastic Surgery, University of Southern California Keck School of Medicine, Los Angeles, CA, USA; 5Department of Plastic Surgery, Medstar Georgetown University Hospital, Washington, DC, USA; 6Department of Surgery, Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ, USA
Correspondence to: Michael Sosin, M.D. Department of Surgery, Medstar Georgetown University Hospital, 3800 Reservoir Road, NW, 4th Floor Pasquerilla Health Center, Washington, DC 20007, USA. Email: [email protected].
Background: Currently, there is a lack of clear guidelines regarding evaluation and management of giant juvenile fibroadenomas. The purpose of this study was to conduct a systematic review of giant juvenile fibroadenomas and to evaluate the most common diagnostic and therapeutic modalities.
Methods: A systematic literature search of PubMed and MEDLINE databases was conducted in February 2014 to identify articles related to giant juvenile fibroadenomas. Pooled outcomes are reported.
Results: Fifty-two articles (153 patients) met inclusion criteria. Mean age was 16.7 years old, with a mean lesion size of 11.2 cm. Most patients (86%) presented with a single breast mass. Imaging modalities included ultrasound in 72.5% and mammography in 26.1% of cases. Tissue diagnosis was obtained using a core needle biopsy in 18.3% of cases, fine-needle aspiration (FNA) in 25.5%, and excisional biopsy in 11.1% of patients. Surgical treatment was implemented in 98.7% of patients (mean time to treatment of 9.5 months, range, 3 days to 7 years). Surgical intervention included excision in all cases, of which four were mastectomies. Breast reconstruction was completed in 17.6% of cases. There were no postoperative complications.
Conclusions:
Diagnosis and treatment of giant juvenile fibroadenoma is heterogeneous. There is a paucity of data to support observation and non-operative treatment. The most common diagnostic modalities include core needle or excisional biopsy. The mainstay of treatment is complete excision with an emphasis on preserving the developing breast parenchyma and nipple areolar complex. Breast reconstruction is uncommon, but may be necessary in certain cases.
Submitted Apr 22, 2015. Accepted for publication May 28, 2015.
doi: 10.3978/j.issn.2227-684X.2015.06.04