If You Remove Mesh For Any Reason, Do You send to Pathology or send to the Trash (May.2019)
Review of Literature
Clinical Value of Hernia Mesh Pathology Evaluation
Presented at the Annual Scientific Meeting of the American College of Surgeons Southern California Chapter, Santa Barbara, CA, January 2019.
Negin Fadaee, AA
, Laura Mazer, MD, Rajeev Sharma, MD Isabel Capati, RN, BSNd
, Bonnie Balzer, MD, PhDc
, Shirin Towfigh, MD, FACSd,∗,’Correspondence information about the author MD, FACS Shirin TowfighEmail the author MD, FACS Shirin Towfigh
Background
Hernia mesh removal is growing in demand. Meanwhile, there is no standard for handling the mesh specimen or any consensus on the clinical value of the surgical pathology findings.
Study Design
All hernia mesh specimens gathered from 2013 to 2018 were analyzed. Patients were categorized based on indication for mesh removal. The “mesh reaction” group included those with clinical reaction deemed to be related to the mesh material. The “mesh nonreaction” group included patients who had mesh removed for a clinical indication unrelated to the mesh material.
Results
One hundred and one patients had 115 mesh specimens that were microscopically evaluated. Patients with clinical diagnosis of mesh reaction were significantly younger (39 vs 56 years; p = 0.023) and more likely to be female (71% vs 39%; p < 0.001) than those without mesh reaction. Although the clinical symptoms were significantly different, the pathology findings were quite similar.
Conclussion
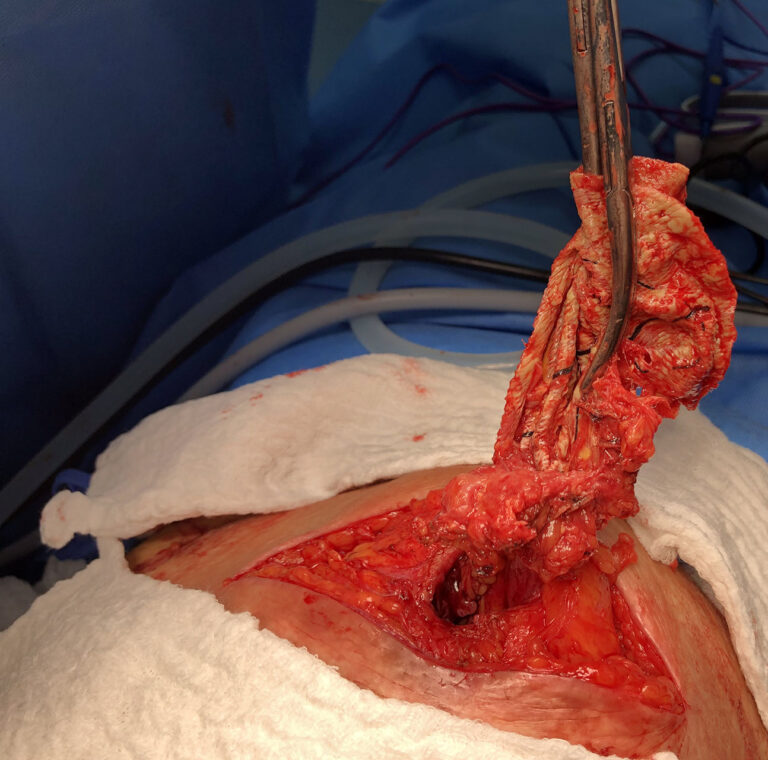
There is no clinical value in submitting mesh specimens for microscopic surgical pathology evaluation, regardless of clinical indication for the mesh removal. Also, no clinical claims can be made based on pathology findings from explanted mesh. In addition, microscopic evaluation does incur additional costs to the consumer. We recommend explanted mesh be submitted for gross examination only for documentation purposes in the medical records.
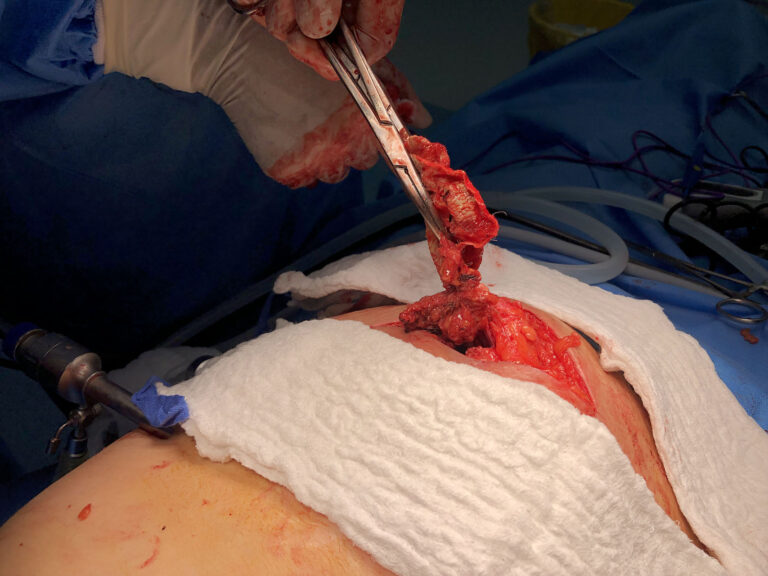
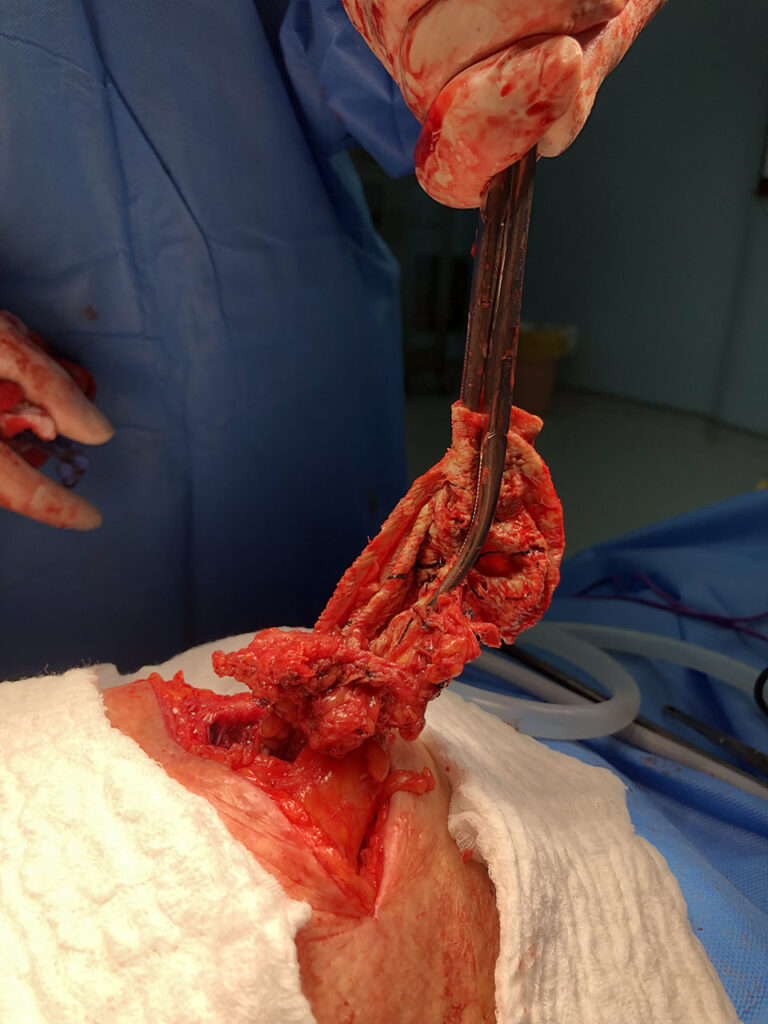
Mesh removal is necessary in a subset of patients who have undergone hernia repair. The indications for mesh removal are varied and include infection, chronic pain (eg due to meshoma, nerve entrapment, or mesh erosion), and incidental removal (eg at the time of recurrent hernia repair or unrelated operation).1, 2 A rare indication for mesh removal is serious allergic, immunogenic, or inflammatory reaction to the mesh product itself. We term these as mesh reactions.
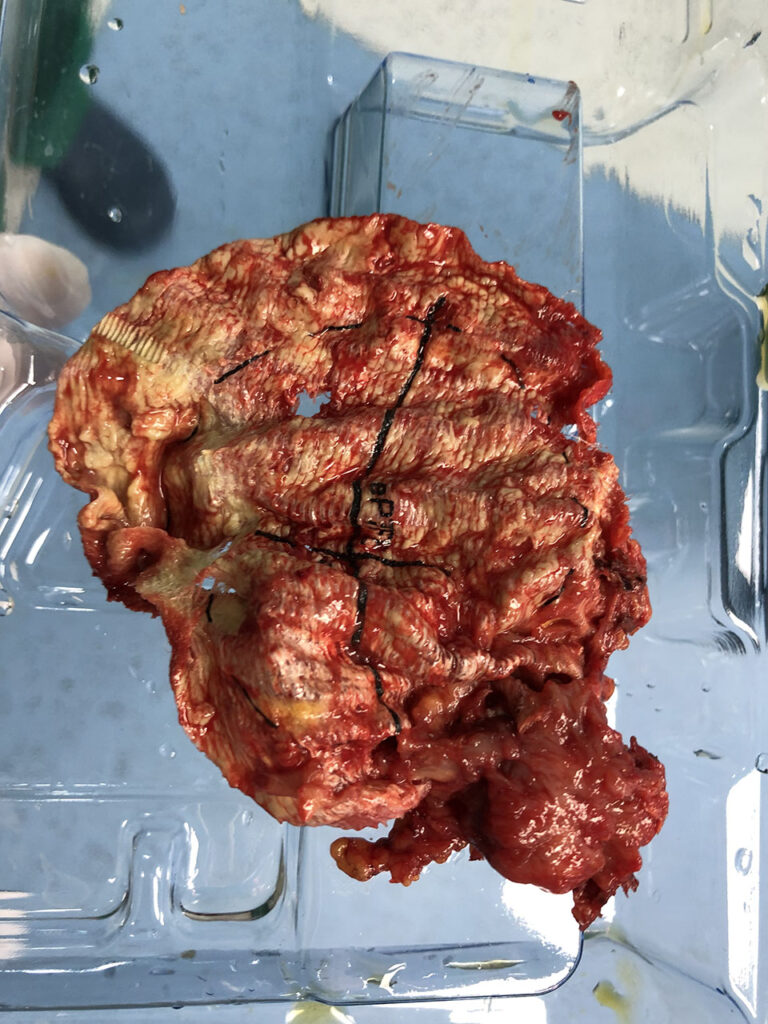
Microscopic examination of hernia mesh shows an array of foreign-body reactions in the adjacent tissue.3, 4 What has not yet been shown is the clinical value of these pathology findings. As a result, there is currently no standard as to whether explanted mesh should be sent to surgical pathology for microscopic evaluation. Also, it is unclear if any clinical deductions can be made from the pathology findings or whether these findings would change clinical management of the patient.
Meanwhile, we are seeing a surge in the number of patients who are seeking to have their mesh removed. This is reflected not only in our clinical practice, but also in lay discussions in online forums and social media. On Twitter, for example, the term #mesh has been tagged more than 180,000 times and #meshremoval has been tagged 1,500 times in the past year alone, resulting in close to 250,000,000 potential views on this subject.5 On the patient discussion board, HerniaTalk.com, there are more than 500 posts specifically discussing mesh removal.6 Patients seeking medicolegal consultation are required to have their mesh sent to surgical pathology as “potentially unique and important evidence.”7
To date, there is no standard as to how to handle the mesh specimen. In an online survey of international hernia surgeons, there was no standard practice on the handling of mesh specimens—70% sent mesh for gross examination only, 7% sent their specimen for microscopic evaluation, and 20% discarded the specimen.