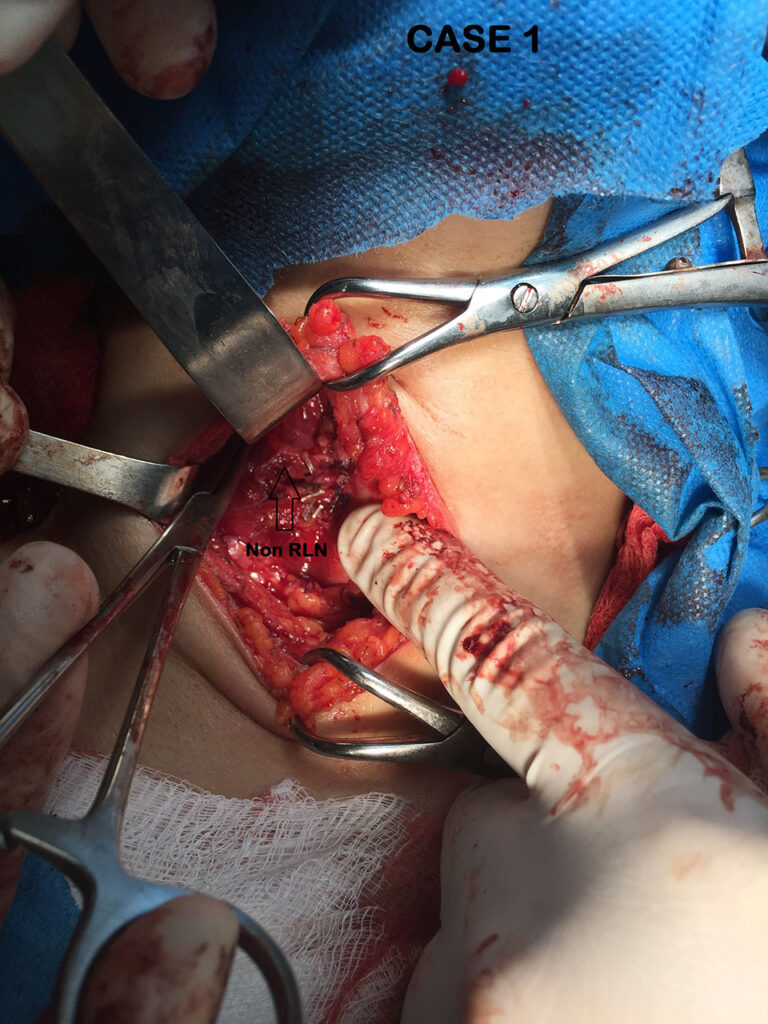
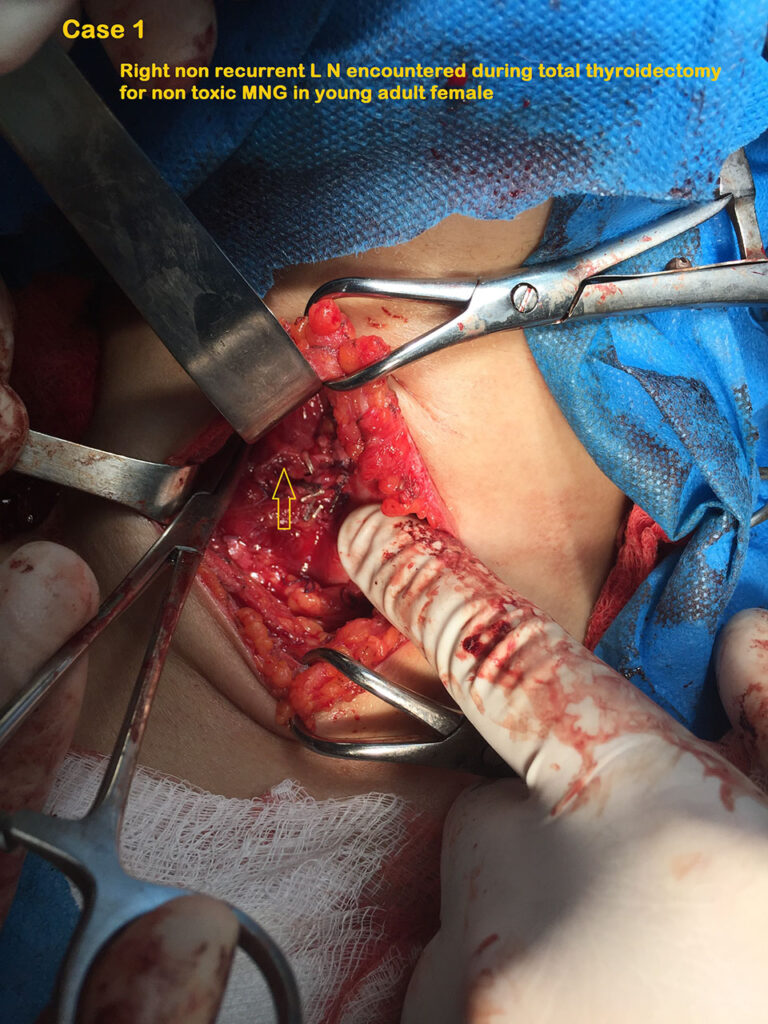
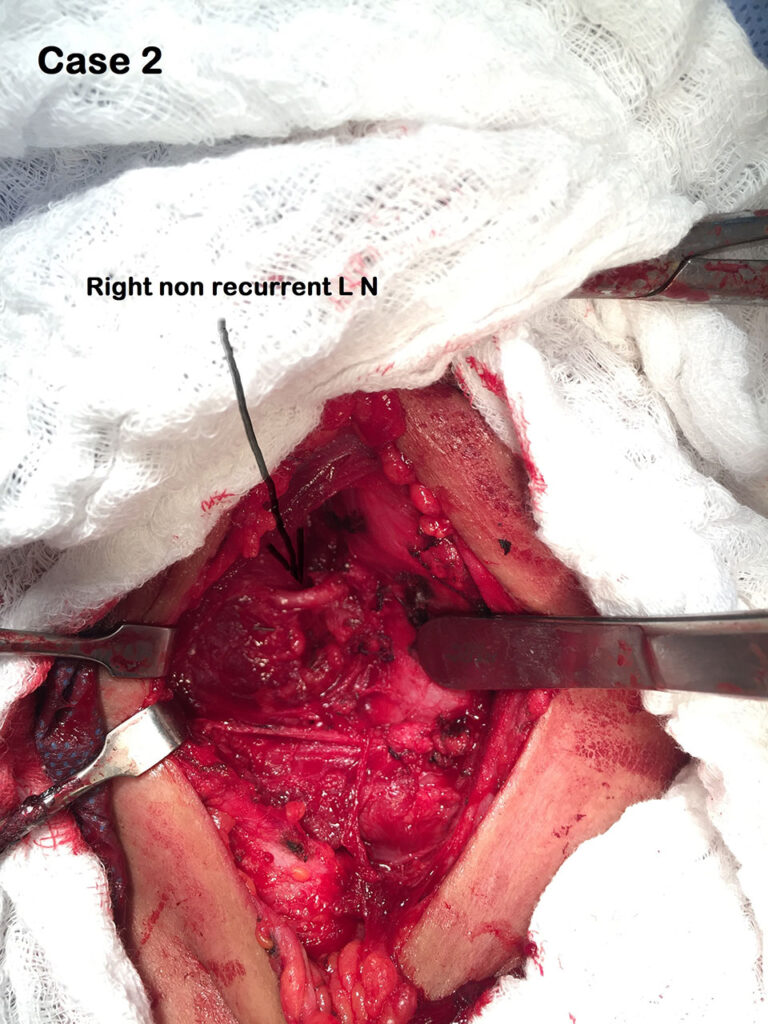
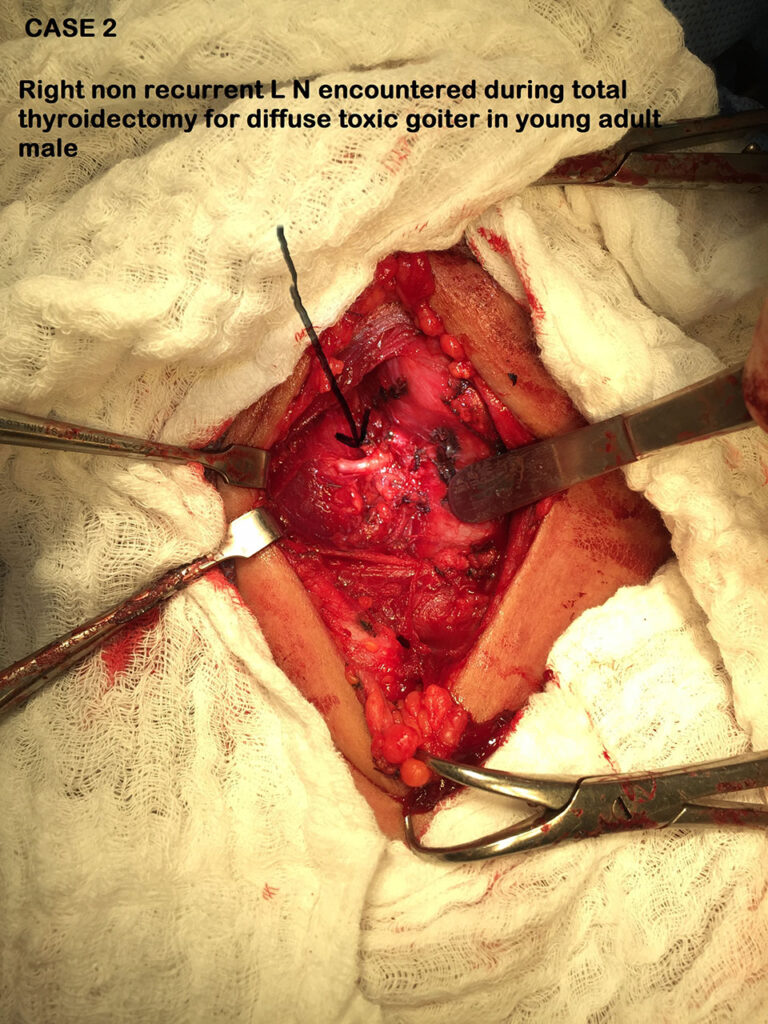
Non Recurrent Laryngeal Nerve encountered during total thyroidectomy (Jan. 2018)
Review Of Literatures
Identifying the Non-recurrent Laryngeal Nerve: Preventing a Major Risk of Morbidity During Thyroidectomy
Rahim Mahmodlou, Mohammad Reza Aghasi,1 and Nariman Sepehrvand2
Author information ► Article notes ► Copyright and License information ►
This article has been cited by other articles in PMC.
Abstract
Non-recurrent laryngeal nerve (NRLN) is a rare anomaly which is reported in 0.3%-0.8% of people on the right side and in 0.004% (extremely rare) on the left side. Damage to this nerve during the surgical procedure may lead to severe iatrogenic morbidity and should therefore be prevented from being damaged. The best way to avoid this damage to the nerve is to identify the nerve with a systematic diligent dissection based on usual anatomical landmarks and awareness about the possibility of their existence. Hereby, we are going to present a 26-year-old woman, a case of NRLN on the right side which was identified during thyroidectomy. The nervous anomaly was accompanied with vascular abnormality which was confirmed by computerized tomography (CT) angiography, post-operatively.
Keywords: Inferior laryngeal nerve, non-recurrent, thyroidectomy
PeerJ. 2017; 5: e3012.
Published online 2017 Mar 21. doi: 10.7717/peerj.3012
PMCID: PMC5363258
The Non-Recurrent Laryngeal Nerve: a meta-analysis and clinical considerations
Brandon Michael Henry,corresponding author1,2 Silvia Sanna,3 Matthew J. Graves,1,2 Jens Vikse,2,4 Beatrice Sanna,5 Iwona M. Tomaszewska,6 R. Shane Tubbs,7 Jerzy A. Walocha,1,2 and Krzysztof A. Tomaszewski1,2
Academic Editor: M. Fabiana Kubke
Author information ► Article notes ► Copyright and License information ►
Abstract
Background
The Non-Recurrent Laryngeal Nerve (NRLN) is a rare embryologically-derived variant of the Recurrent Laryngeal Nerve (RLN). The presence of an NRLN significantly increases the risk of iatrogenic injury and operative complications. Our aim was to provide a comprehensive meta-analysis of the overall prevalence of the NRLN, its origin, and its association with an aberrant subclavian artery.
Methods
Through March 2016, a database search was performed of PubMed, CNKI, ScienceDirect, EMBASE, BIOSIS, SciELO, and Web of Science. The references in the included articles were also extensively searched. At least two reviewers judged eligibility and assessed and extracted articles. MetaXL was used for analysis, with all pooled prevalence rates calculated using a random effects model. Heterogeneity among the included studies was assessed using the Chi2 test and the I2 statistic.
Results
Fifty-three studies (33,571 right RLNs) reported data on the prevalence of a right NRLN. The pooled prevalence estimate was 0.7% (95% CI [0.6–0.9]). The NRLN was found to originate from the vagus nerve at or above the laryngotracheal junction in 58.3% and below it in 41.7%. A right NRLN was associated with an aberrant subclavian artery in 86.7% of cases.
Conclusion
The NRLN is a rare yet very clinically relevant structure for surgeons and is associated with increased risk of iatrogenic injury, most often leading to temporary or permanent vocal cord paralysis. A thorough understanding of the prevalence, origin, and associated pathologies is vital for preventing injuries and complications.
Keywords : Arteria lusoria, Recurrent Laryngeal Nerve, Meta-analysis, Non-Recurrent Laryngeal Nerve, Anatomy.