Solid Pancreatic Pseudopapillary Tumor Managed Laparoscopically (May 2018)
Case presentation
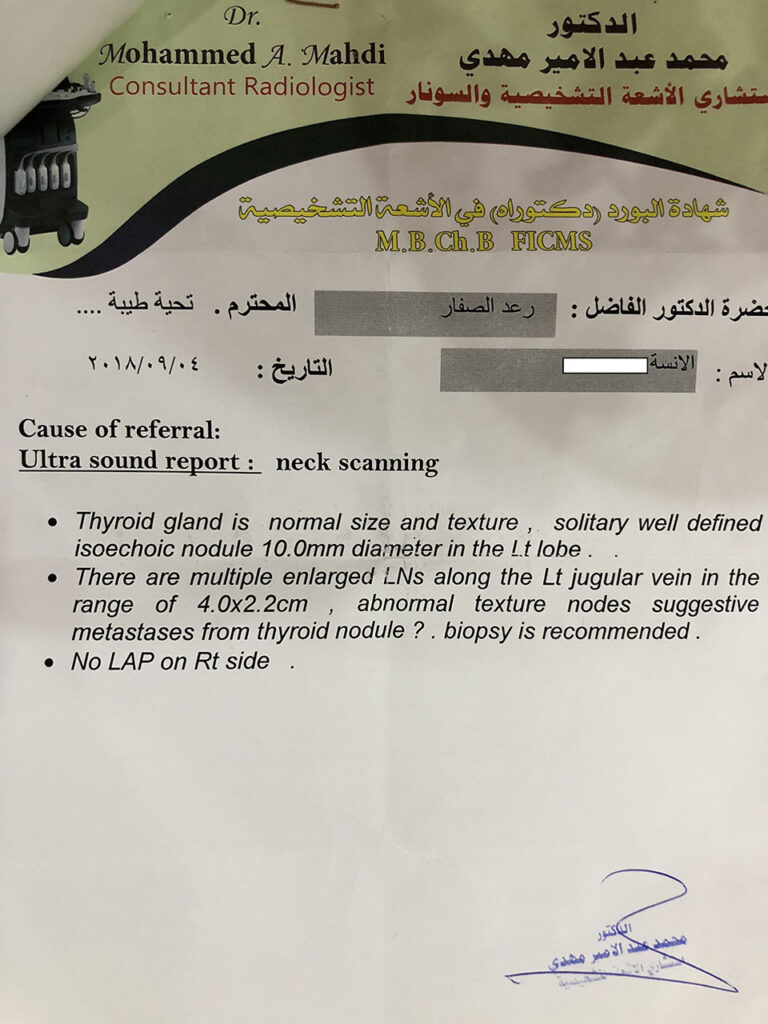
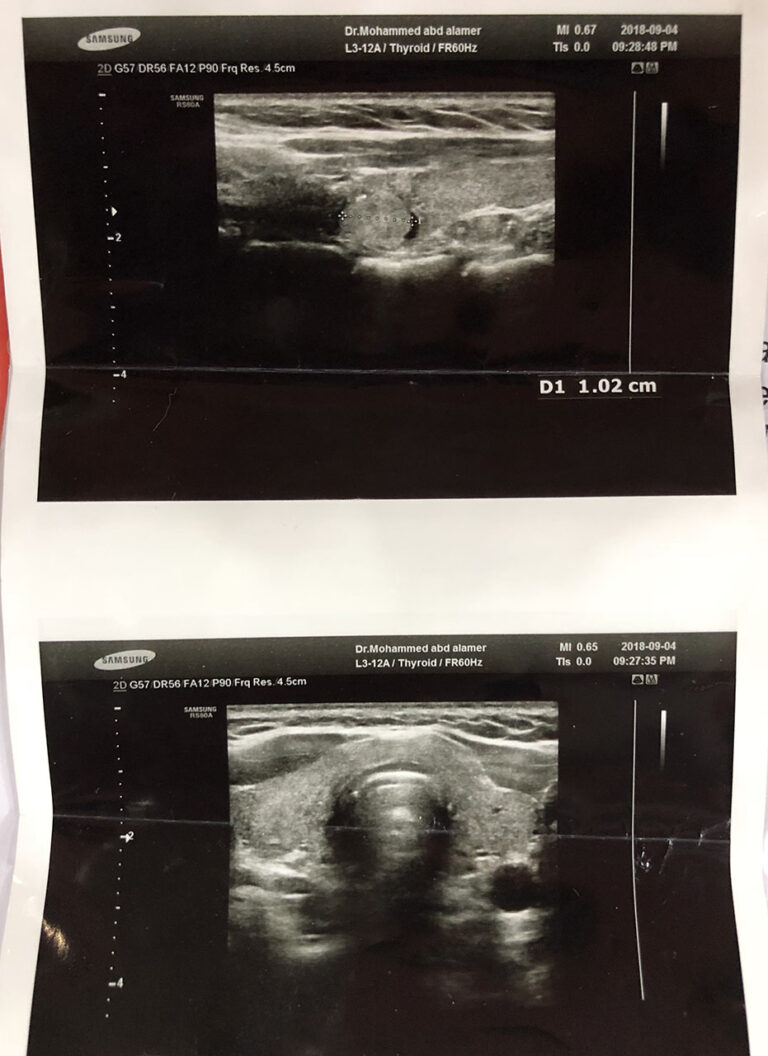
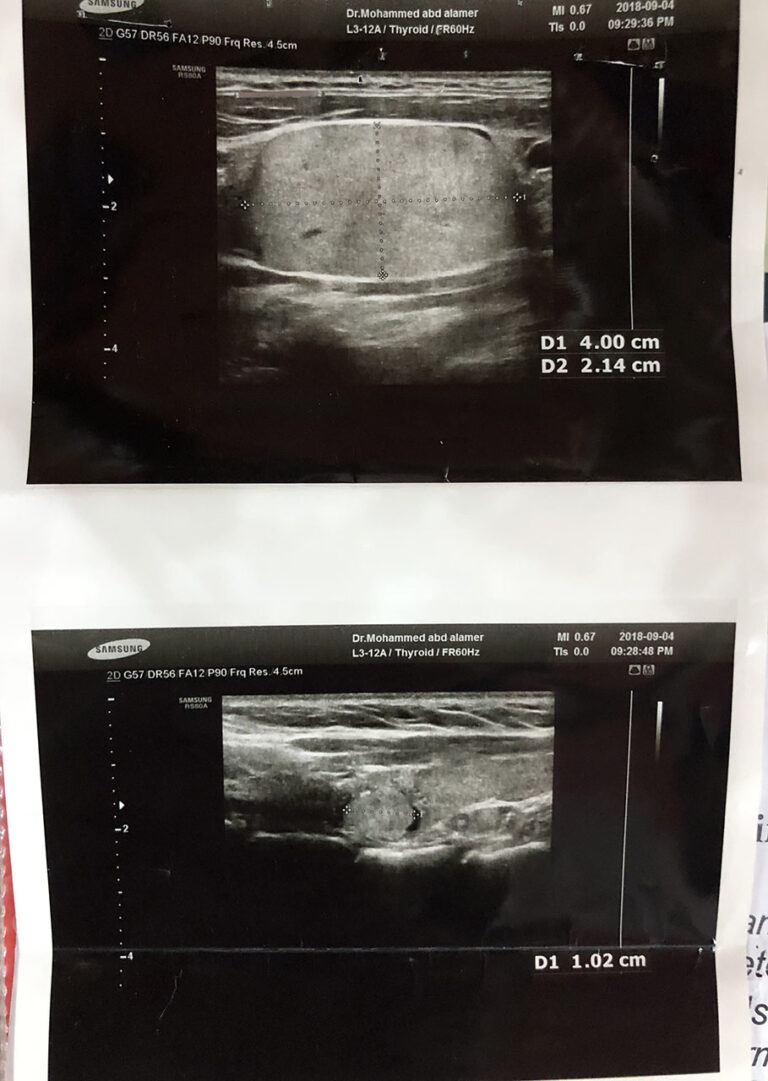
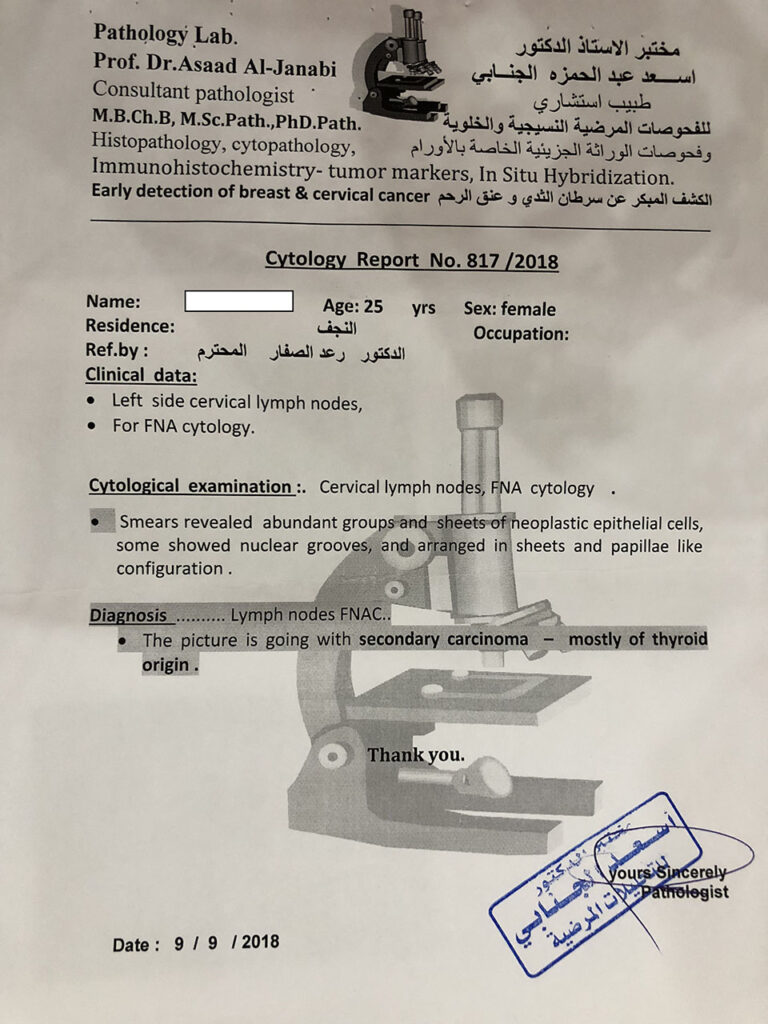
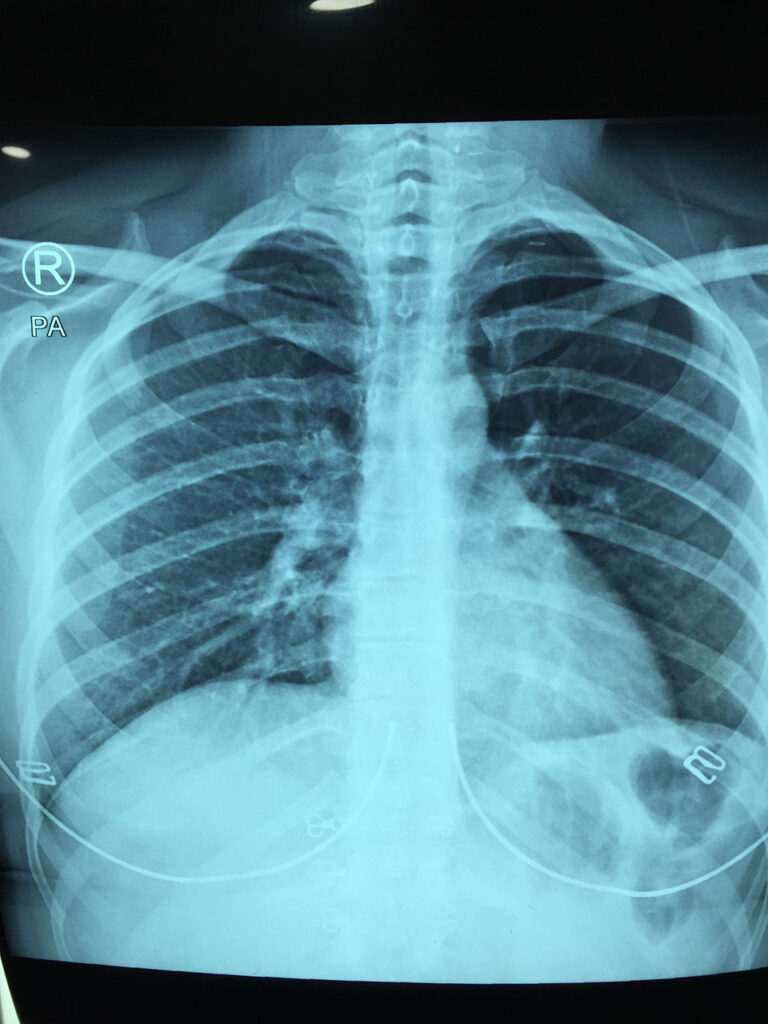
25 years old female patient presented with painless left cervical lymph node enlargement for one month duration not responding to simple medical treatment. On examination there were multiple enlarged and palpable firm left upper, middle and lower jugular lymph nodes with palpable solid left thyroid nodule.Neck ultrasound examination with chest x ray done followed by FNAC from cervical LN.
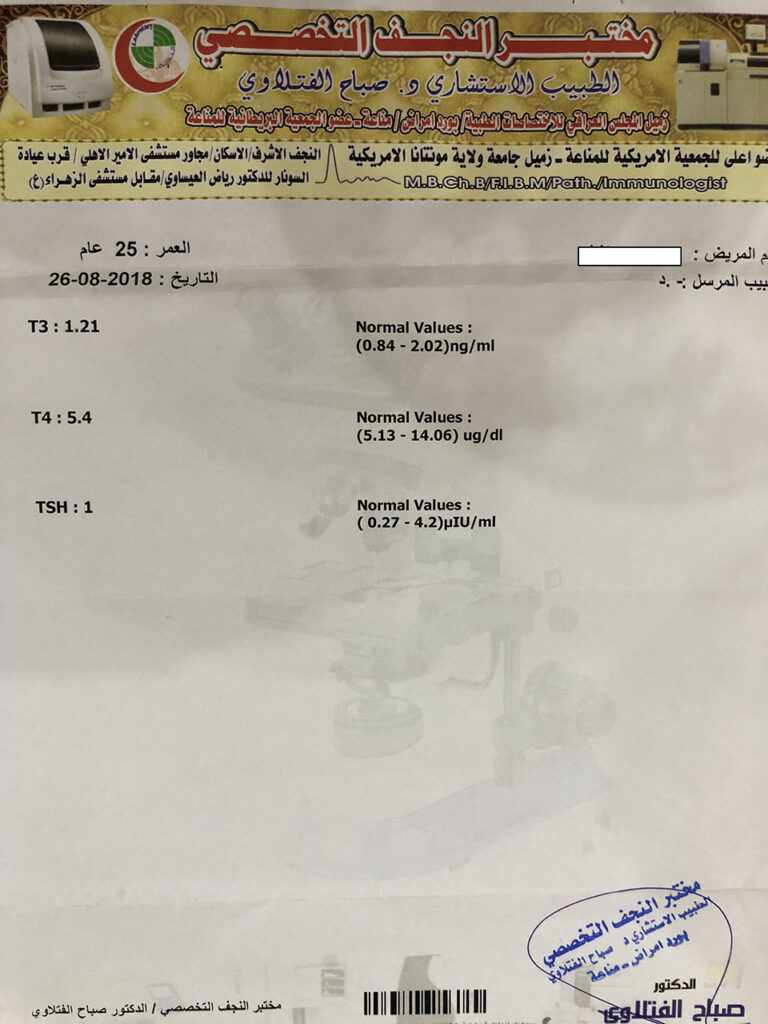
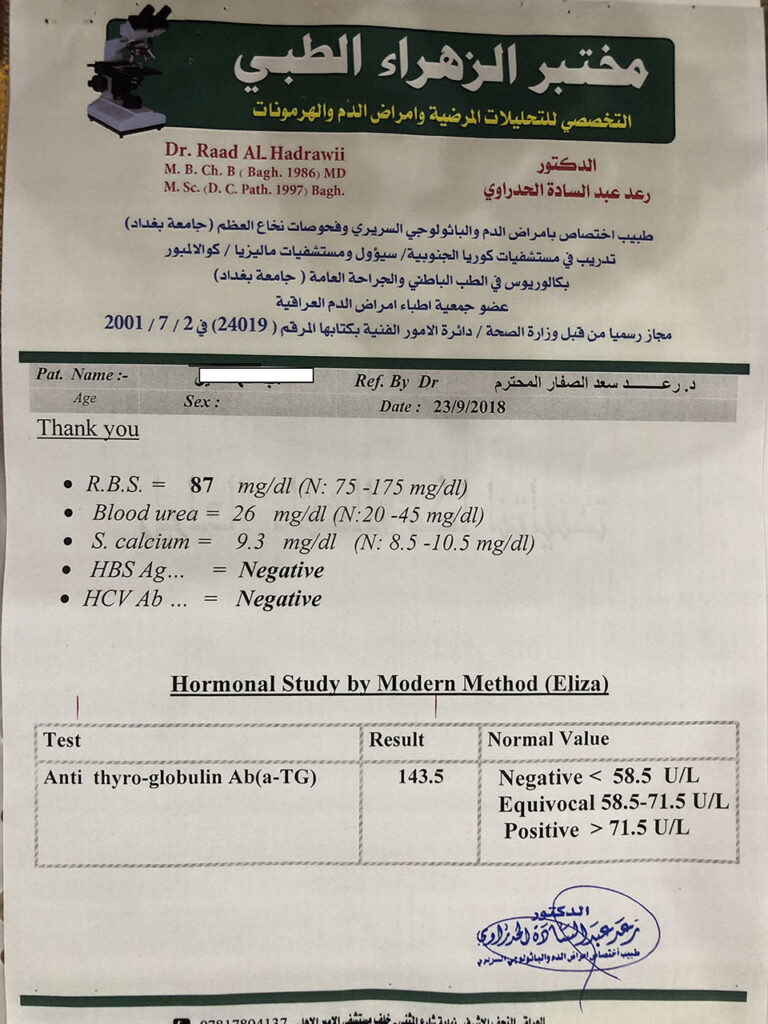
Thyroid function test was normal.
DIAGONSIS was thyroid carcinoma with metastasis to cervical LNs.
The patient prepared for surgery.
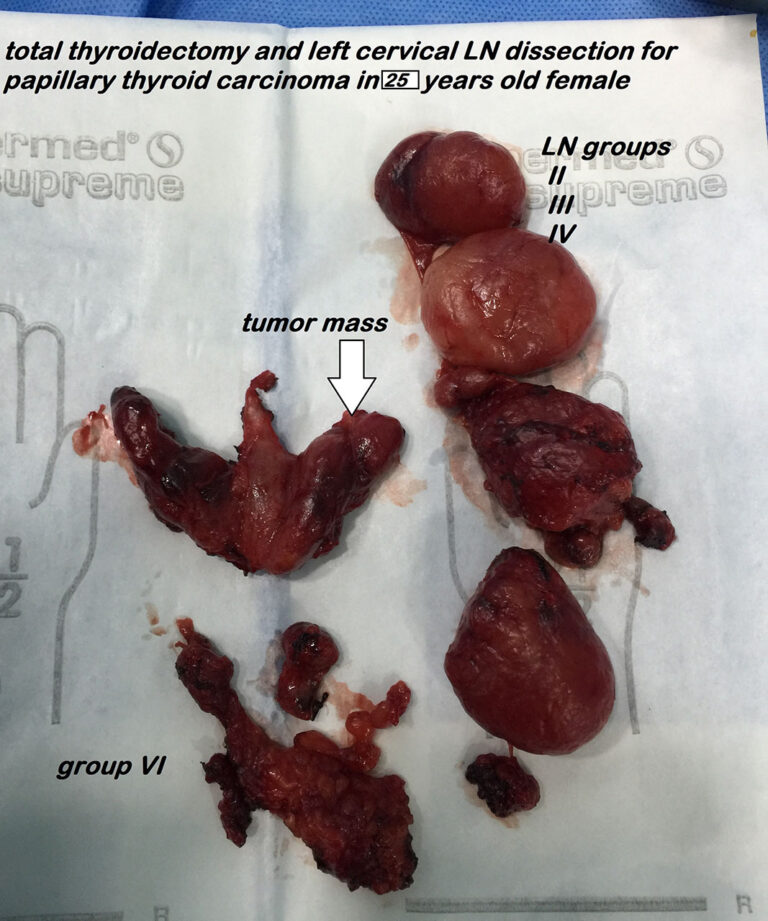
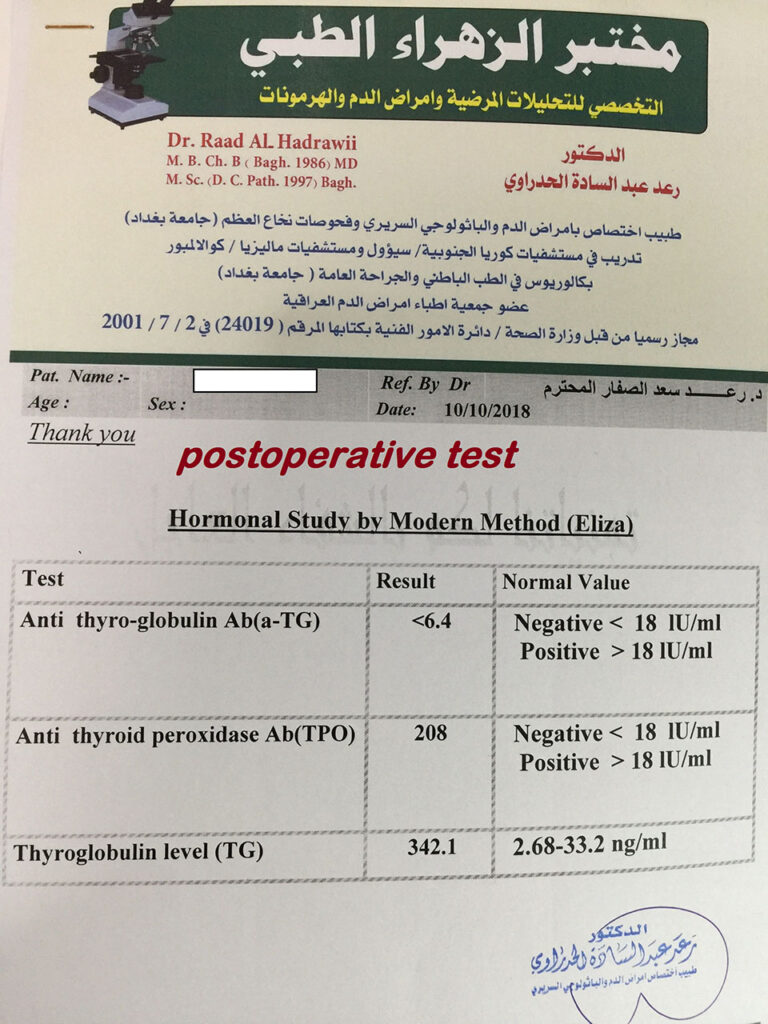
The operation done: total thyroidectomy with selective left cervical LNs dissection plus central group LNs dissection. There was smooth postoperative course {neither recurrent LN injury nor hypoparathyroidism happened}.
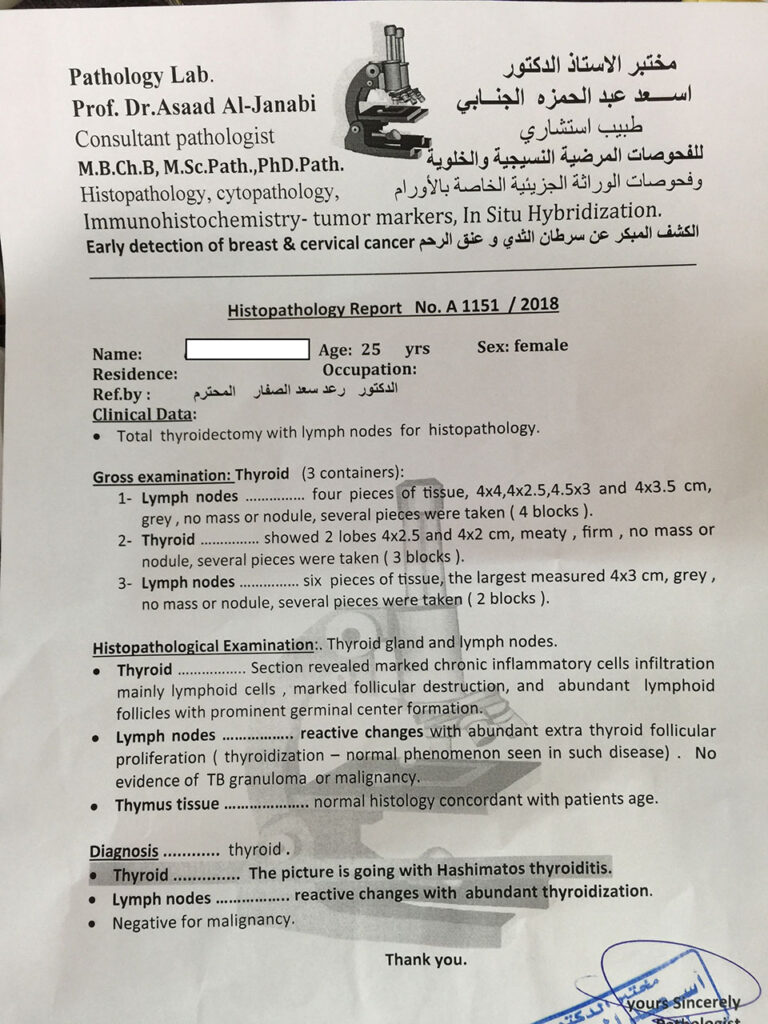
First histopathological report mentioned Hashimoto’s thyroiditis with abundant thyroidization of lymph nodes !!!
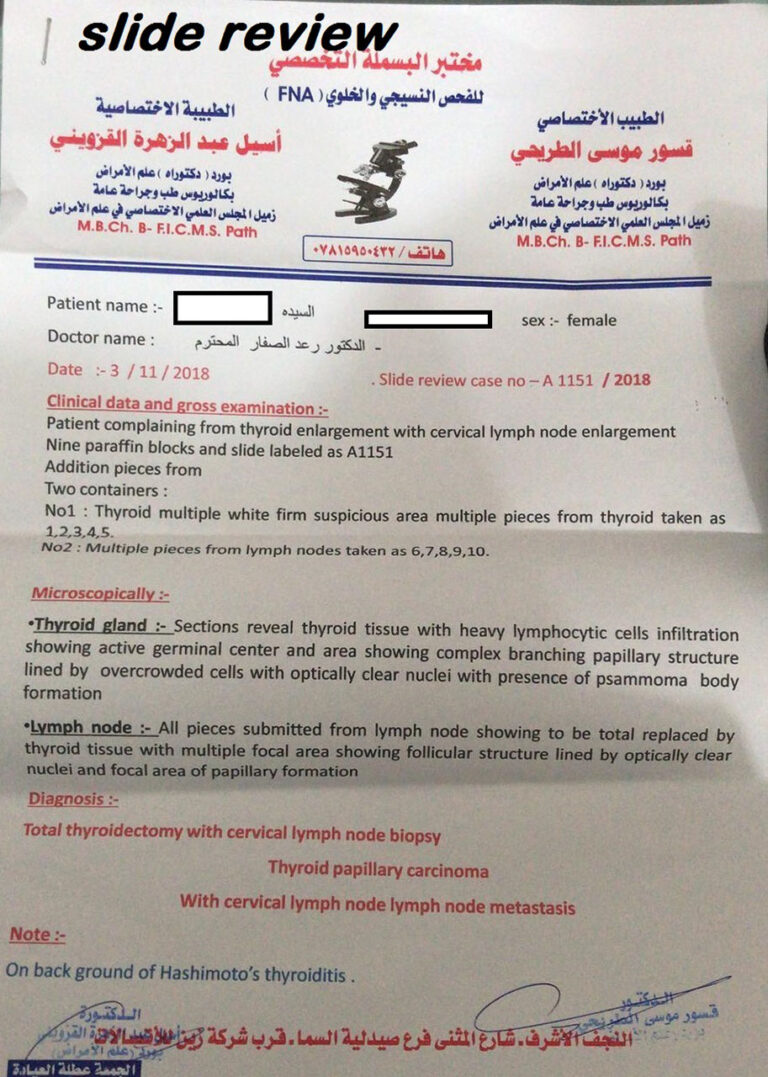
Slide review done and the final report was thyroid papillary carcinoma with multiple lymph nodes metastasis.
Pattern and Distribution of Lymph Node Metastases in Papillary Thyroid Cancer
Hossam A El-Foll1, Hesham I El-Sebaey2, Ahmad F El-Kased1, Ali Hendawy3 and Mahmoud M Kamel4*
1Department of Surgical Oncology, Faculty of Medicine, Menofia University, Egypt
2Department of Surgical Oncology, National Cancer Institute, Cairo University, Egypt
3Department of Surgical Pathology, Faculty of Medicine, Cairo University, Egypt
4Department of Clinical Pathology, National Cancer Institute, Cairo University, Egypt
Abstract
Background: The indications and extent of lymph node dissection in the treatment of papillary thyroid carcinoma remains controversial, and benefit from therapy is debatable. This study was designed to identify the pattern and distribution of lymph node metastases and to establish an optimal strategy for neck dissection for those patients.
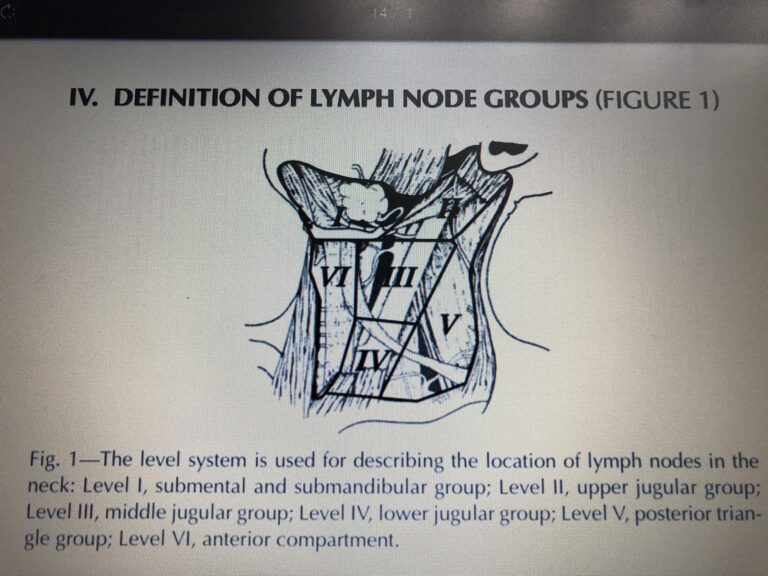
Methods: A total of 44 patients diagnosed with papillary thyroid cancer were treated from 2006 to 2013. All patients underwent total thyroidectomy, central neck dissection, and ipsilateral selective neck dissection removing lymphatic structures in levels II through V. The frequency of cervical lymph node metastases in each level, and the presence of capsular invasion were analysed. In addition, we investigated postoperative complications after total thyroidectomy and central lymph node dissection.
Results: Lymph node metastases were found in 18 patients (40.9%); all of them had ipsilateral level VI nodal involvement. 7 patients had level V involvement, 2 patients had level II affection, 3 patients had level III & IV affection and 2 patients had contralateral level VI lymph node affection. We also found extracapsular invasion in 6 (13.6%) patients and grade I, II, III in 2, 40, 2 patients respectively. The frequency of temporary hypocalcaemia, permanent hypocalcaemia and temporary vocal cord paralysis were 6.8%, 2.3% and 4.5%, respectively.
Conclusion: We recommend total thyroidectomy and central compartment lymph node dissection. If ipsilateral central lymph nodes are positive for metastases in frozen section, we proceed to ipsilateral selective neck dissection removing lymphatic structures in levels II through V even in the absence of clinically evident lymph node metastasis irrespective of tumor size. The technique had a low rate of complications; namely laryngeal nerve injury and hypoparathyroidism.
Keywords
Papillary thyroid carcinoma; Total thyroidectomy; Lymph node metastases; Neck dissection