Unusual presentation of type IV Choledochal cyst in 8 years old boy (Des. 2018)
Case presentation
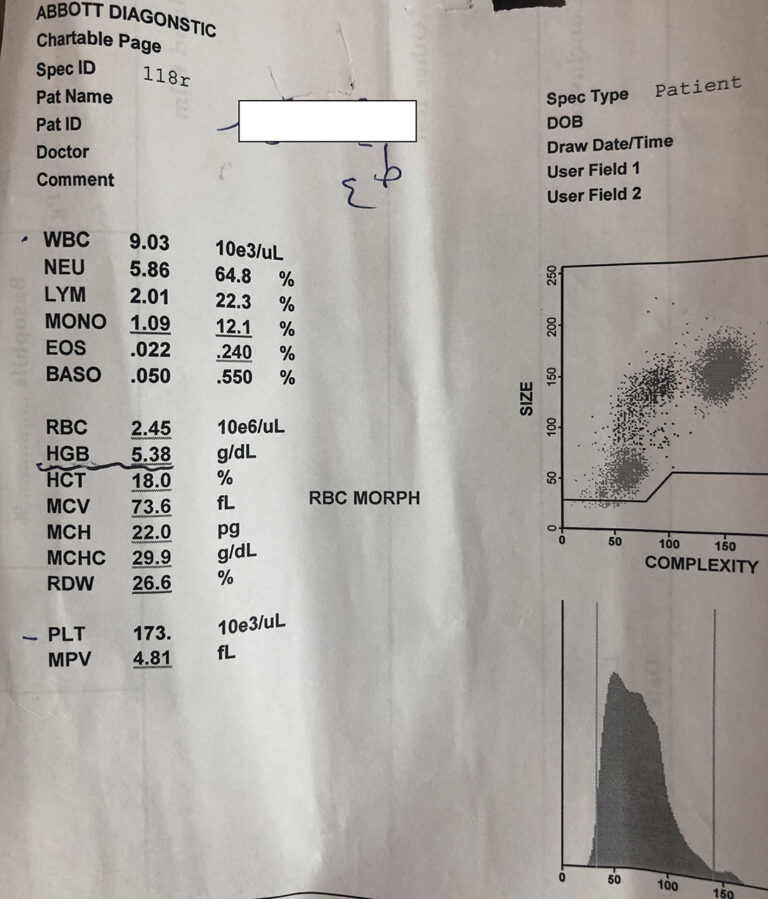
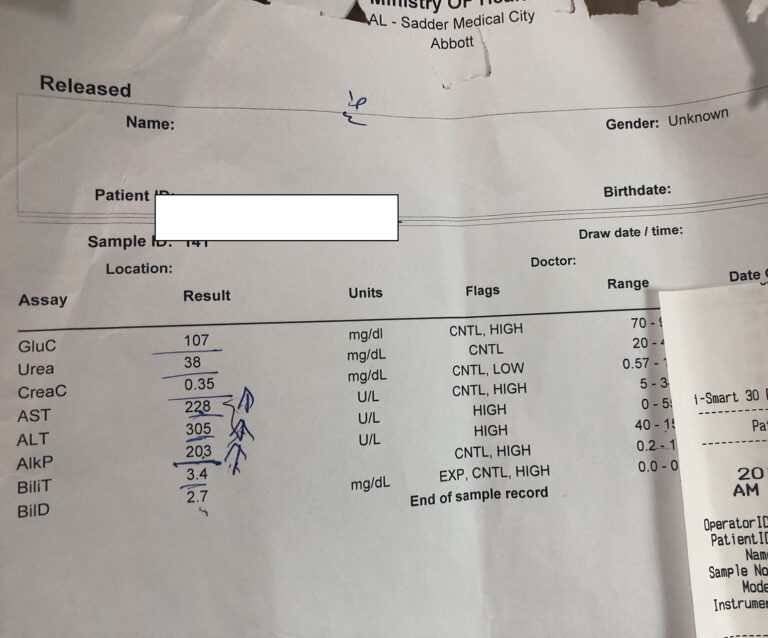
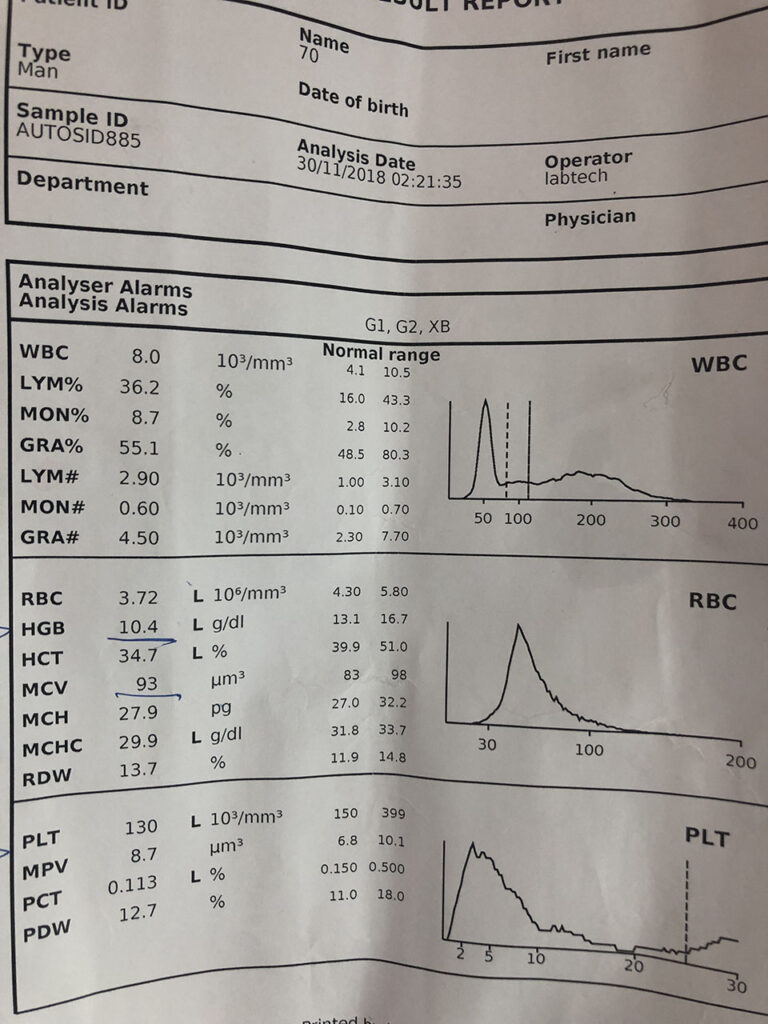
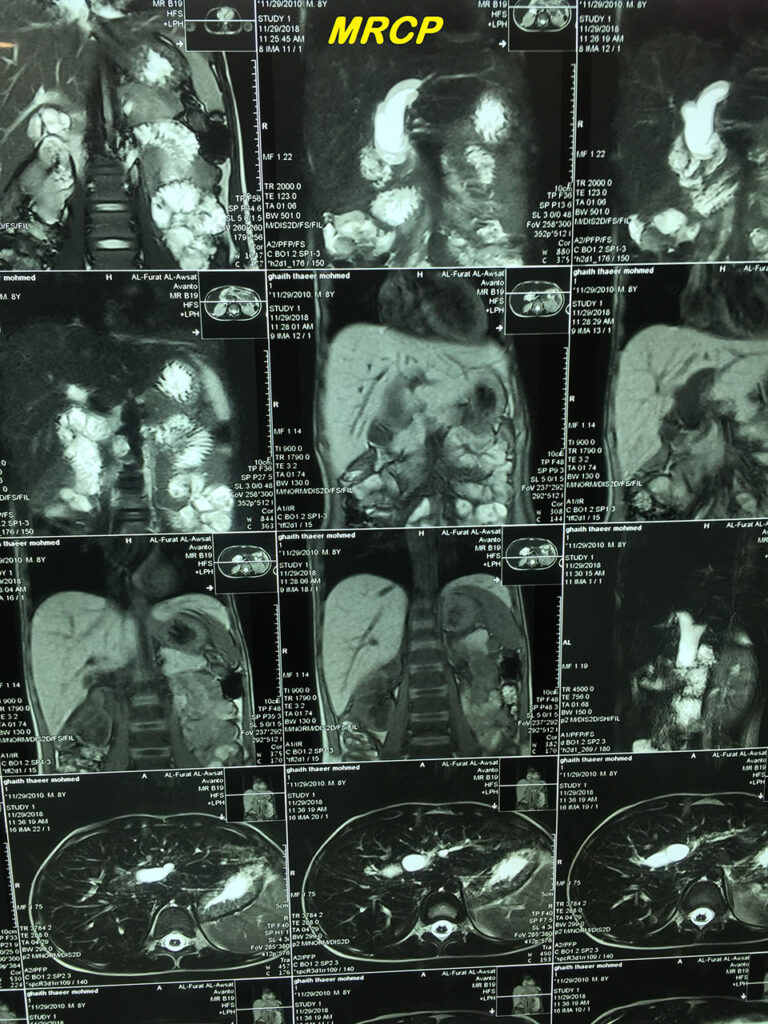
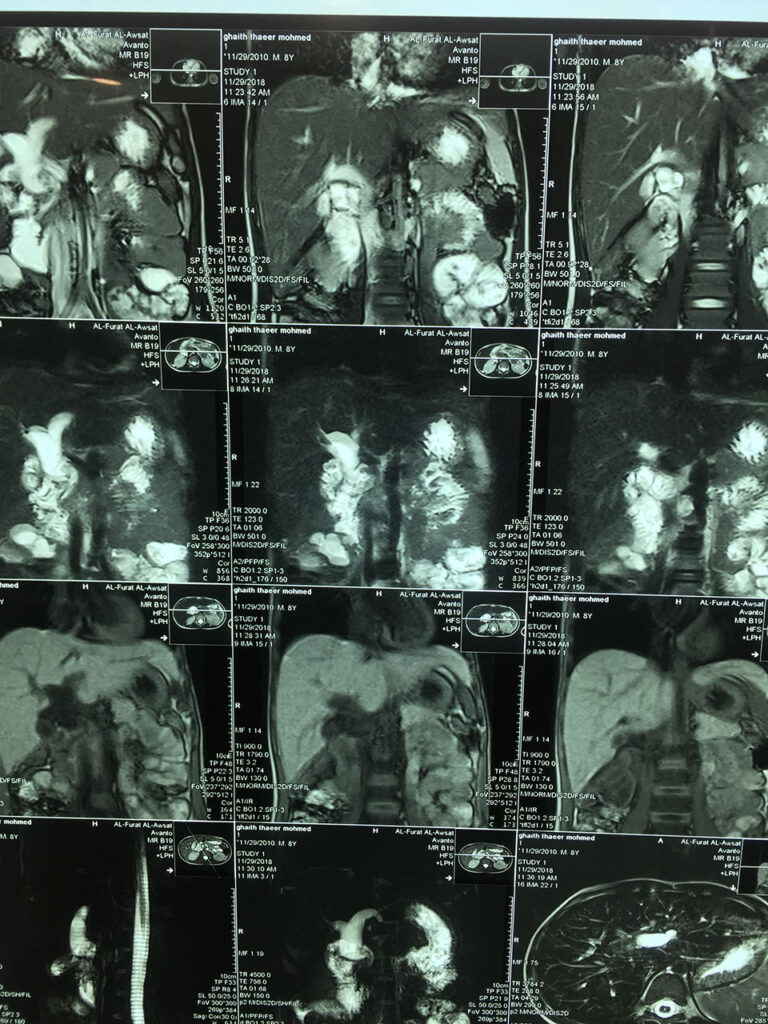
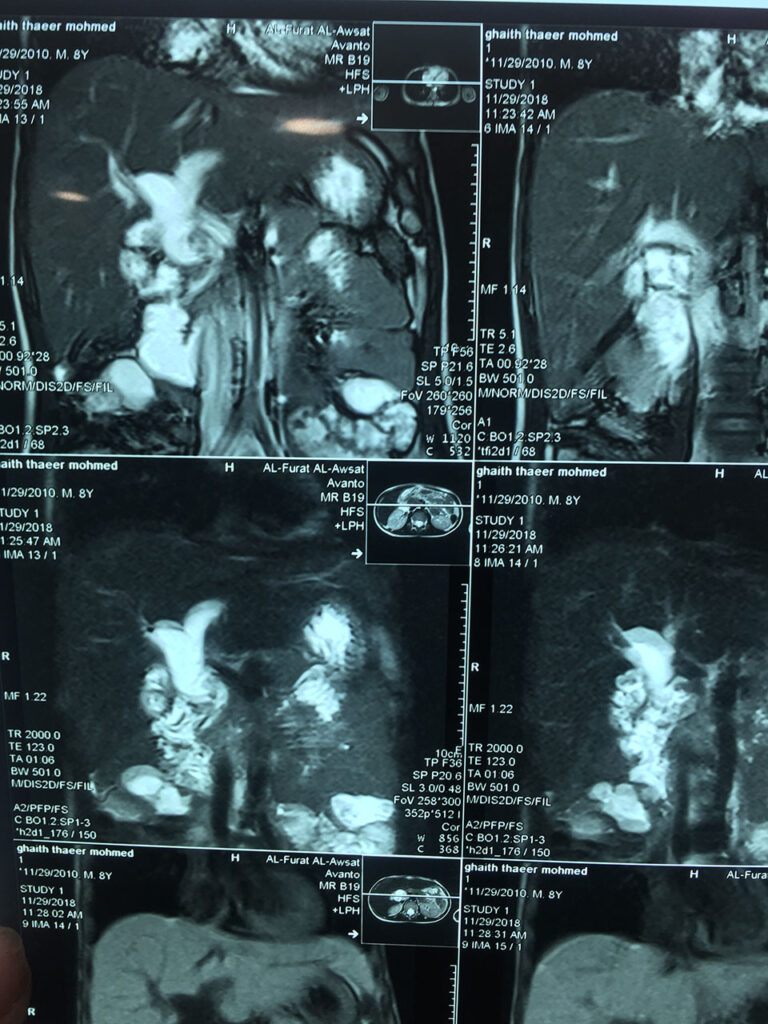
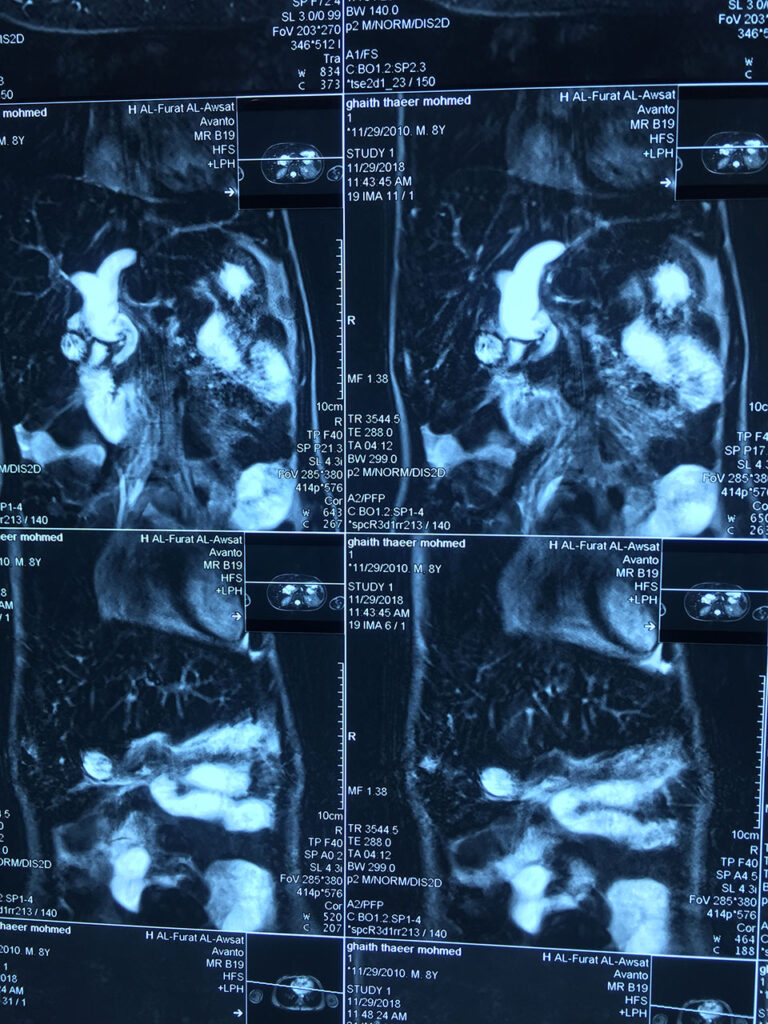
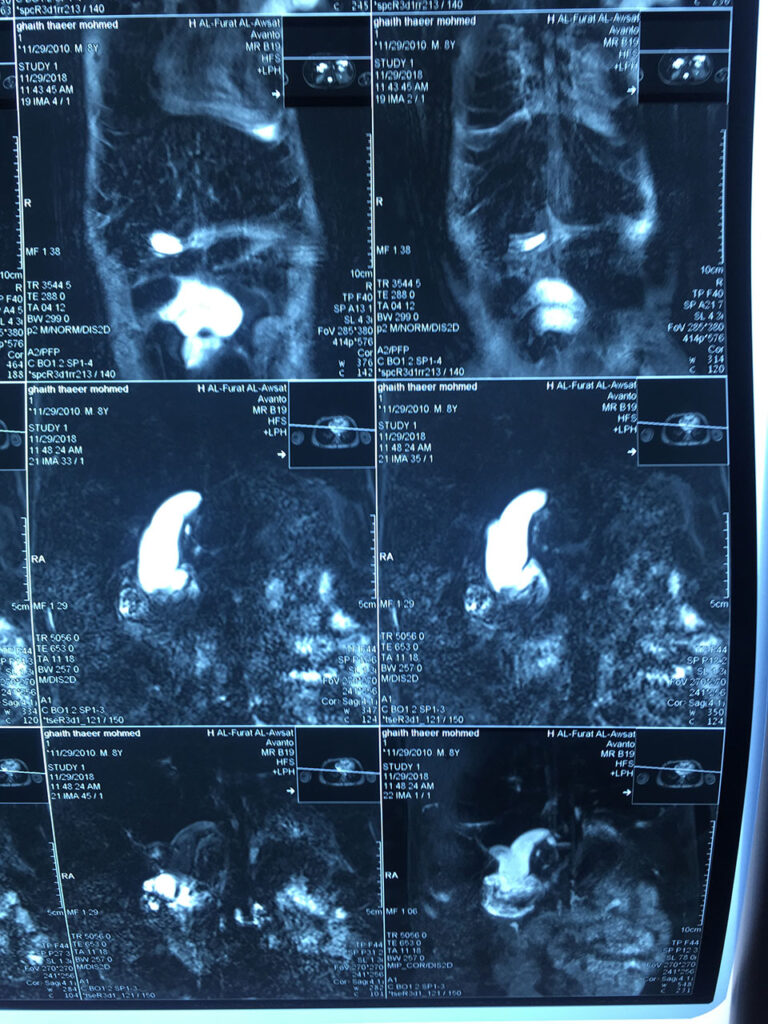
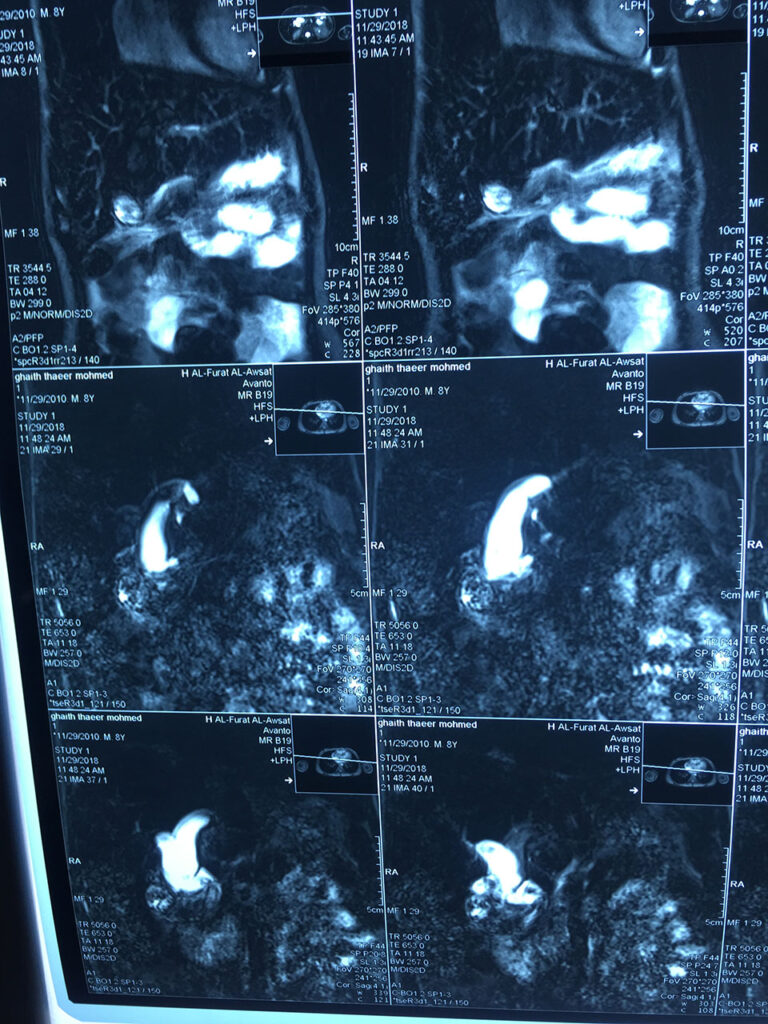
Eight years old boy referred by the gastroenterologist { Dr Muslim Al Khafagi }, as a case of type IV choledochal cyst for surgical intervention. He was presented with upper GI bleeding and anemia three weeks before referral. He was treated conservatively and emergency OGD was done for him and revealed HAEMOBILIA. Abdominal US and MRI plus MRCP were done. Diagnosis of choledochal cyst was made and referred for operative management.
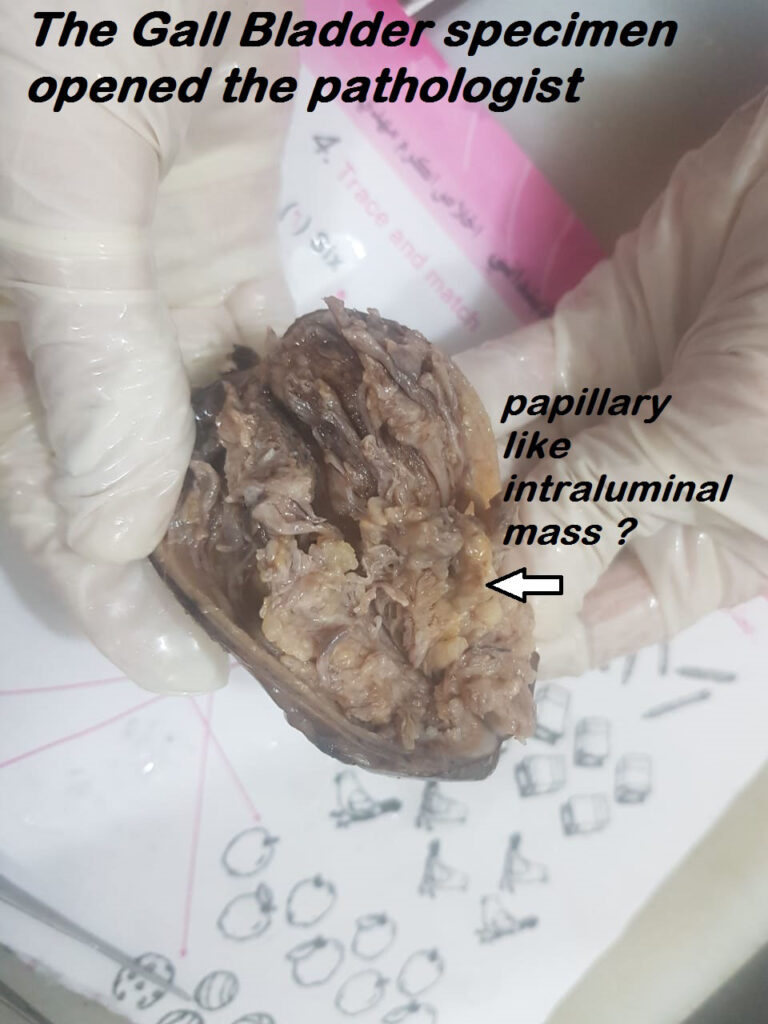
The gastroenterologist thought about possibility of heterotopic gastric tissue in the cyst or in the gall bladder? With ulceration that causing haemobilia!!!
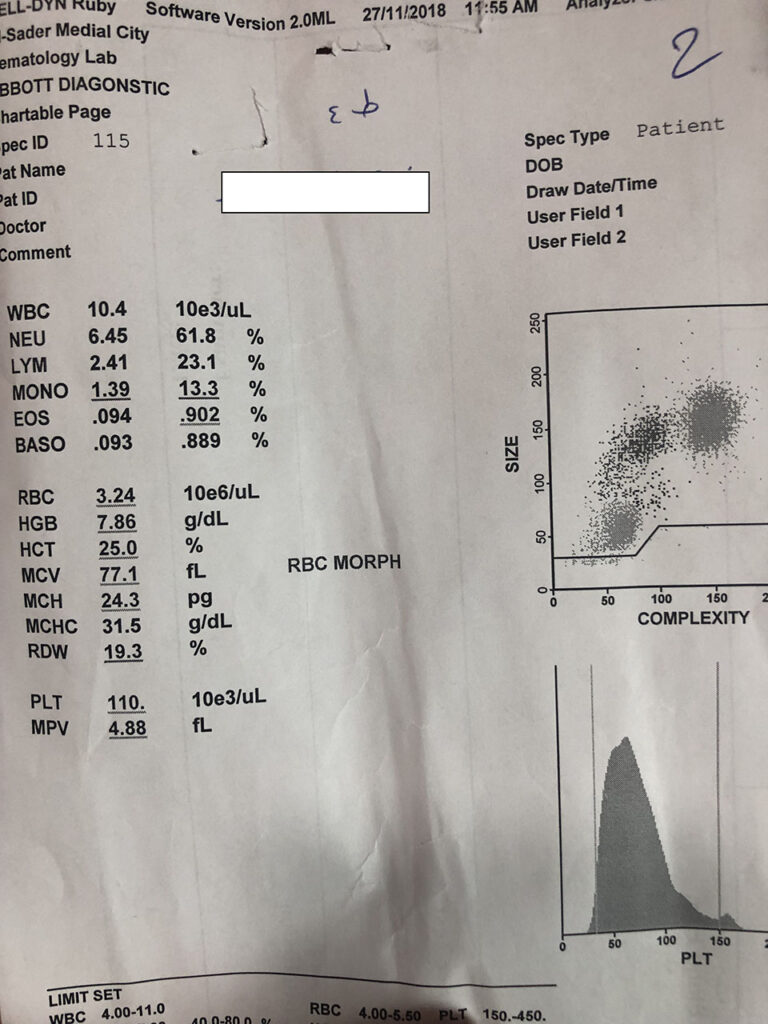
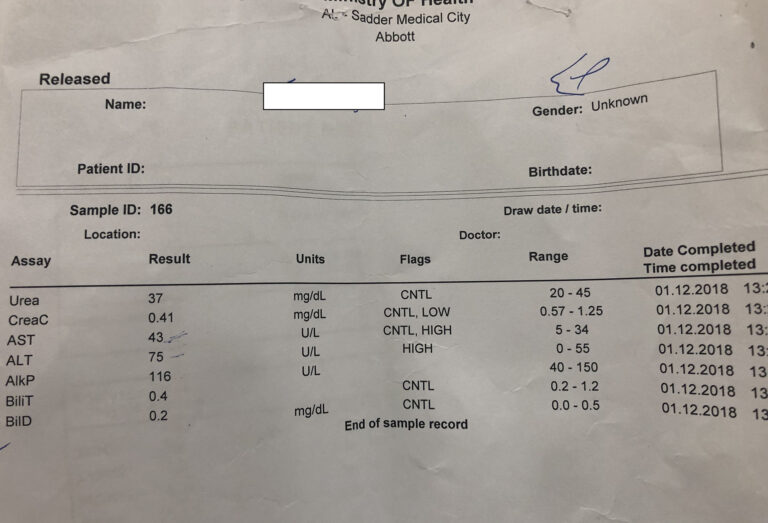
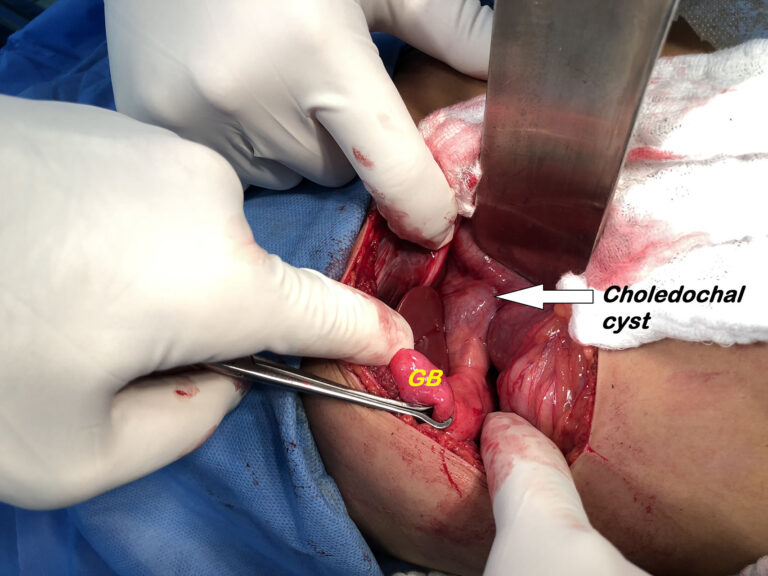
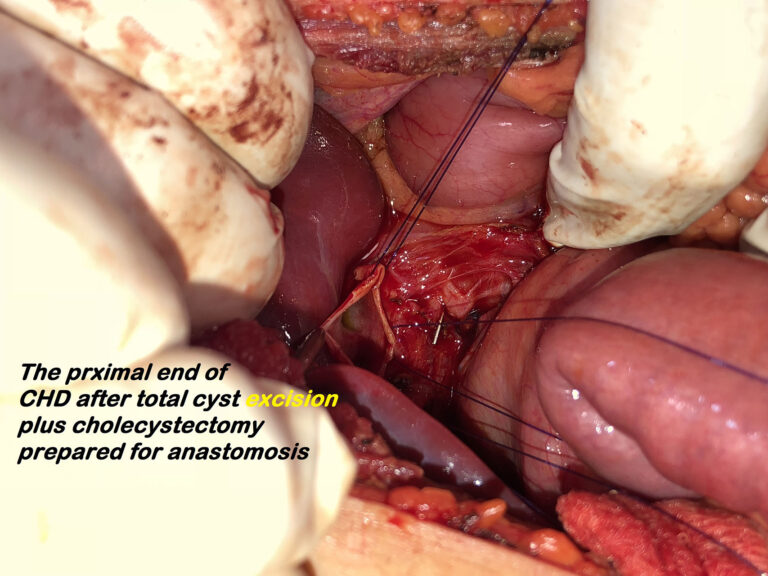
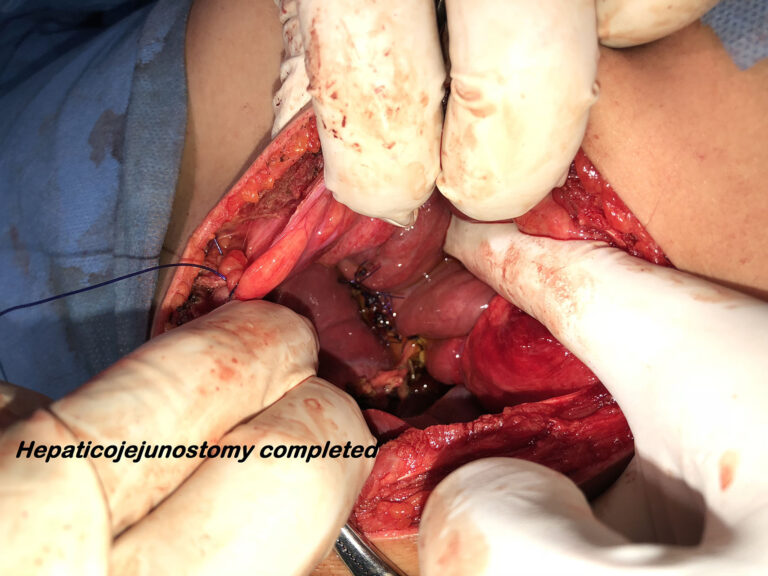
The patient prepared for surgery after blood transfusion. Under general anesthesia , through right subcostal incision the abdomen explored. The operative findings were distended and thick wall gall bladder with type IV choledochal cyst. Cholecystectomy with excision of the cyst was done followed by Roux en Y hepaticojejunostomy. Postoperatively the patient put on intravenous fluid , double intravenous antibiotic and nothing per mouth. He complained from minor bile leak in third postoperative day which stopped after three days .The patient started oral intake in fourth postoperative day. Otherwise the postoperative course was smooth and the patient discharged home after one week hospital admission.
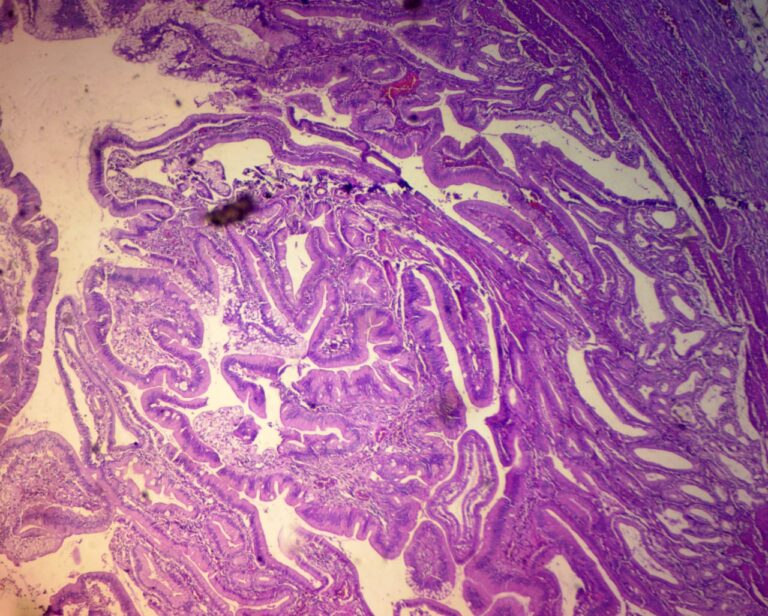
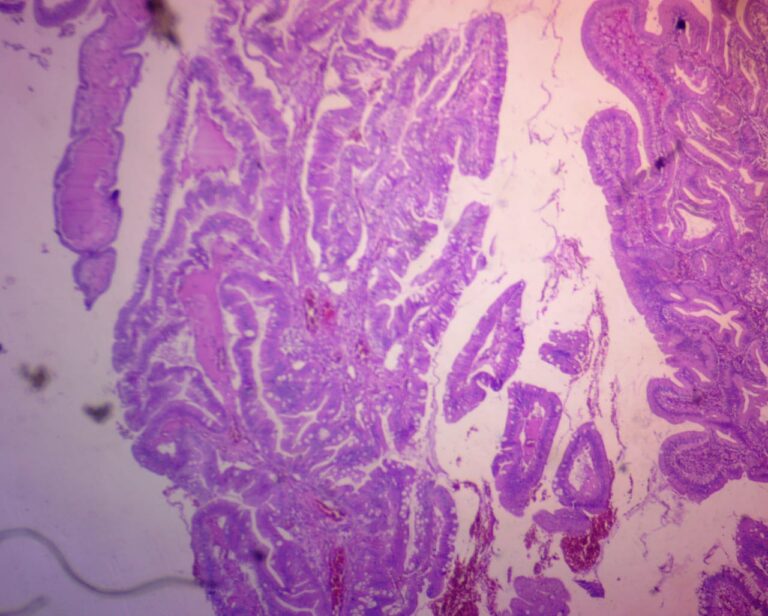
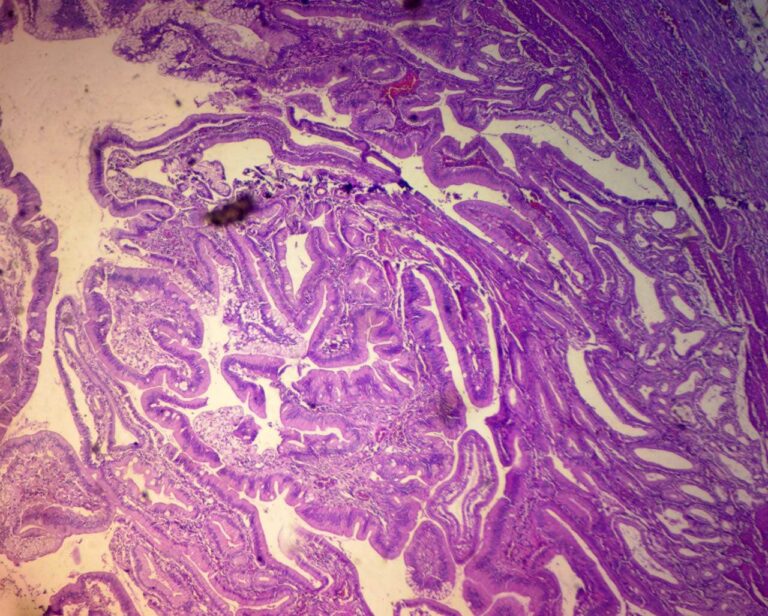
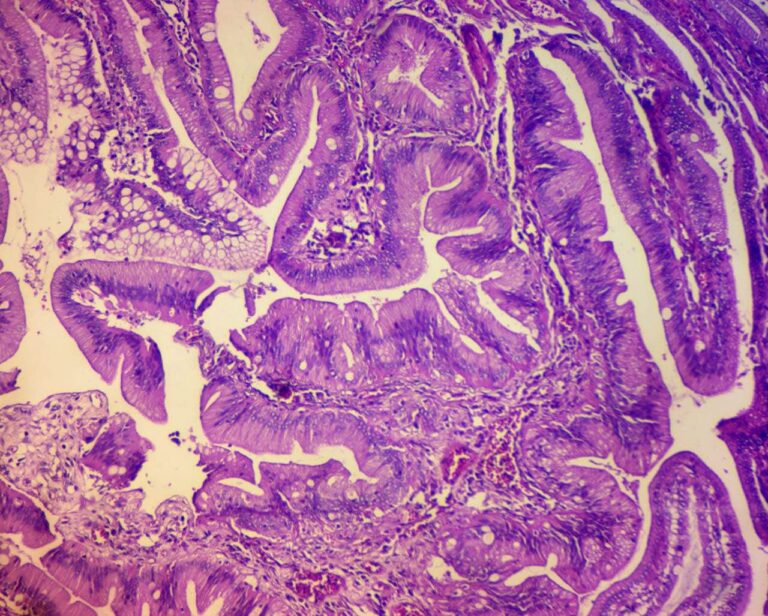
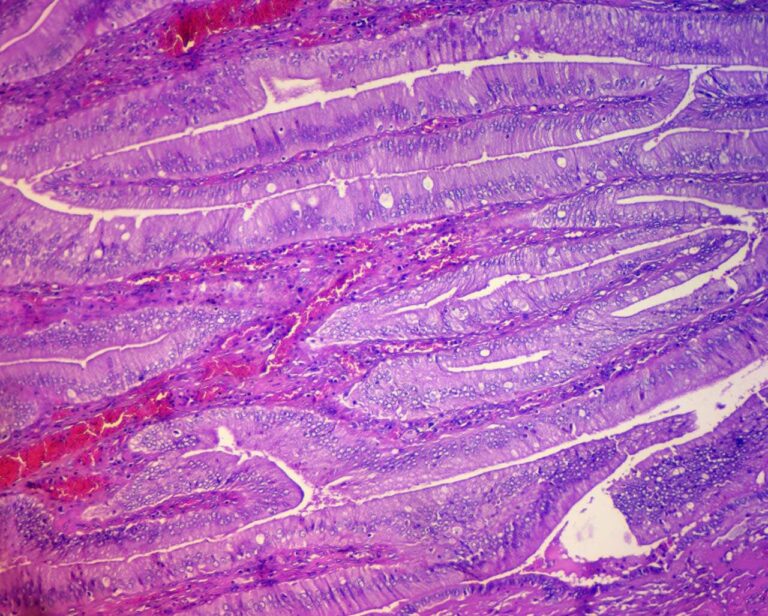
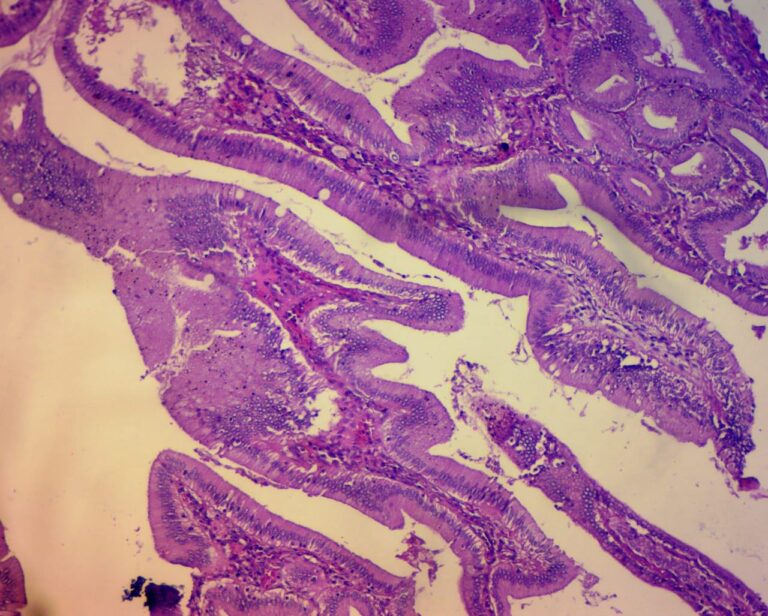
Gall bladder histopathology: Non invasive intracystic papillary tubular neoplasm [ tubulo papillary variant] With intestinal and gastric Favolae metaplasia”
REVIEW OF LITERATURE
Pediatric Choledochal Cyst Surgery
Updated: Mar 22, 2018
Author: Gail E Besner, MD; Chief Editor: Harsh Grewal, MD, FACS, FAAP more…
Background
Cystic dilatation of the common bile duct (CBD), also known as choledochal cyst, is a fairly uncommon anomaly of the biliary tract. Although it was first described by Vater and Ezler in 1723, Douglas published the first complete clinical description of the anomaly in a patient in 1853. He speculated about the congenital nature of this anomaly.In 1959, Alonso-Lej et al published an extensive review of 94 cases in the literature and added two cases of their own. [1] They classified choledochal cysts into three types. In 1977, Todani et al further classified this anomaly into five types. [2] Subsequent subtypes based on cholangiographic findings have been described.
With the use of antenatal ultrasonography, an increasing number of choledochal cysts have been reported in the fetus. [3, 4, 5, 6, 7, 8, 9] Incomplete gastric obstruction by a large cyst is one of the typical clinical manifestations in newborns and young infants. [10] The earliest reported choledochal cyst was detected in a fetus at 15 weeks’ gestation, which may correspond to the timing of the formation of pancreatic enzymes.
Antenatal demonstration of a cystic structure inferior to the liver strongly suggests the diagnosis. Fetal development should be carefully monitored with serial ultrasonography after such a discovery. Most centers prefer to excise the cyst shortly after birth. A waiting period of a few weeks is necessary to stabilize the baby and allow for proper preoperative evaluation. [11] Surgical excision in the neonatal period has been shown to be technically feasible and well tolerated by the patient.
The management of choledochal cysts has evolved during the past several decades. [12] Complete excision of the cyst and biliary bypass have become the treatment of choice. Other procedures, such as cystoduodenostomy or cystojejunostomy, have been associated with high morbidity and the potential for malignant transformation in the residual cyst. Even after complete excision, sporadic cases of cancer in the remaining biliary tree have been reported.
REVIEW OF LITERATURE
Heterotopic Gastric Mucosa in the Gallbladder: A Rare Cause of Massive Hemobilia
Yoon, Angela J*; Cowles, Robert A†; Stylianos, Steven†; O’Toole, Kathleen M*
Journal of Pediatric Gastroenterology and Nutrition: May 2005 – Volume 40 – Issue 5 – p 606-608
Case Report
INTRODUCTION
Hemobilia requiring transfusion is a rare complication of heterotopic gastric mucosa in the gallbladder. Gastric heterotopia in the gallbladder is usually clinically silent and often only discovered incidentally. Symptomatic peptic ulceration of the gallbladder and biliary tree has been reported and may cause pain (1-11). This case report describes the clinical presentation, endoscopic retrograde cholangiopancreatography findings and the histologic features of this rare entity and discusses the possible mechanism leading to hemorrhage.
CASE REPORT
A 17-year-old boy presented with a 5-month history of episodic abdominal pain, nausea, weight loss and bloody stools. There was no history of abdominal trauma. His hematocrit at presentation was 16%. There was moderate elevation of the serum transaminases and alkaline phosphatase. Serum bilirubin was normal. Esophagogastroduodenoscopy and flexible sigmoidoscopy were normal. Because of the abdominal pain and elevated transaminases, a right upper quadrant ultrasound was obtained showing a thickened gallbladder wall with intraluminal debris (Fig. 1). Tc99 pertechnetate radioisotope scan was interpreted as negative for Meckel’s diverticulum. Repeat upper endoscopy with endoscopic ultrasound revealed a thickened gallbladder with echogenic debris. Endoscopic retrograde cholangiopancreatography revealed blood clots emerging from the ampulla of Vater, suggesting hemobilia. Injection of the biliary tree showed multiple obstructing clots in the common bile duct (Fig. 2). A selective hepatic angiogram was performed which was normal. A tagged, red blood cell radioisotope scan failed to localize a bleeding site. Endoscopic cholangioscopy was performed, which suggested that blood was emerging from the left hepatic duct whereas only bile was seen in the right hepatic duct. Based on this observation, angiographic embolization of the left hepatic artery was performed. One week later, the patient returned with recurrent significant gastrointestinal bleeding and a hematocrit of 15%. A repeat angiogram did not reveal a bleeding site. The patient was then taken to the operating room for laparoscopy in search of Meckel’s diverticulum, gastrointestinal duplication or other bleeding site. The small bowel was noted to contain blood. No Meckel’s diverticulum or duplication was discovered. During laparoscopy, the gallbladder was inspected. It was thick-walled with dense, inflammatory adhesions. Based on the grossly abnormal appearance of the gallbladder, laparoscopic cholecystectomy was performed. The patient remained well during the immediate postoperative period with no episodes of bleeding and a stable hematocrit. He was discharged home 7 days after surgery and has had no further bleeding or symptoms for 1 year.